Living with intractable migraine can be incredibly difficult and often debilitating. It is a type of chronic migraine that does not respond to the usual treatments, leaving sufferers in an endless cycle of pain and frustration. Fortunately, there are options available to those living with this condition. In this article, we will explore the causes, symptoms, and potential treatment options for intractable migraine so that you can better understand how to manage your own symptoms. With the right knowledge and care plan in place, you can find relief from your migraines and take back control of your life.
What is Intractable Migraine?
Intractable migraine is a type of chronic migraine that does not respond to any conventional treatment. It is characterized by frequent and intense headaches, usually accompanied by nausea, vomiting, sensitivity to light and sound, and fatigue. These migraines can last 4-72 hours or even longer and can be extremely debilitating for those affected. These migraine flares are usually on a background of daily or near daily headache which may vary and fluctuate in intensity levels continuously day to day.
What can Cause Intractable Migraines?
The exact cause of intractable migraine is still unknown, but several factors may contribute to its development. These include:
- Hormonal changes – Hormonal imbalances such as menopause, pregnancy, or taking certain medications can trigger intractable migraine symptoms.
- Stress – Emotional stress or trauma can lead to an increase in migraine frequency and intensity. Physical stress on the body (such as surgery or injury) can also increase frequency.
- Genetics – Some studies have linked intractable migraine to certain genetic markers.
- Diet – Skipping meals, eating processed foods, or consuming too much caffeine can trigger migraines.
- Environmental factors – Exposure to bright lights, loud noises, strong smells, or changes in barometric pressure can bring on a migraine attack.
What Risk Factors can Affect the Development of Intractable Migraines?
Certain risk factors may increase your likelihood of developing intractable migraine, such as:
- Age – Intractable migraines are most common among those between the ages of 25 and 55.
- Gender – Women are more likely to suffer from intractable migraine than men.
- Family history – If you have a family history of chronic migraine, you may be more prone to developing intractable migraine.
- Medical conditions – People with certain medical conditions, such as depression or anxiety, may also be at an increased risk for intractable migraine.
- Medication overuse headache (rebound headache) – If acute (abortive) medications are being used excessively (over the counter pain medicines, triptans, butalbital, opiates), this will sustain and worsen chronic intractable migraine indefinitely until the overuse pattern stops. After excessively used medications are weaned off, headaches will often worsen (rebound) before they improve during the wean, and this process can take 4-6 weeks.
- Head injury – People with a head injury such as a concussion, brain surgery, or traumatic brain injury can develop a daily headache which often resembles a chronic intractable migraine.
Symptoms of Intractable Migraine
The primary symptom of intractable migraine is intense and frequent headaches lasting from 4-72 hours or longer, on top of a daily or near daily headache which may vary and fluctuate in intensity levels continuously day to day.
Common Symptoms of Intractable Migraine
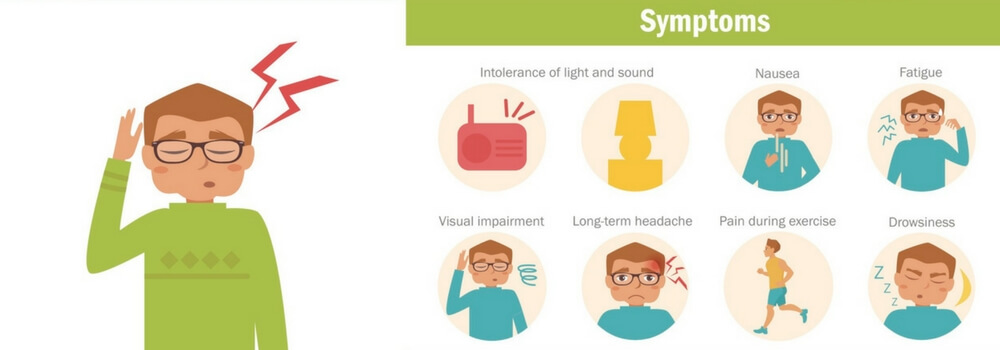
The symptoms of intractable migraine can vary from person to person, but common symptoms include intense and frequent headaches lasting from 4-72 hours or longer. These headaches are often accompanied by nausea, vomiting, sensitivity to light and sound, and fatigue. Some people may also experience dizziness, blurred vision, difficulty concentrating, confusion, irritability, depression and anxiety. In addition to these physical symptoms, sufferers may also experience a feeling of pressure behind the eyes or in the temples as well as sensitivity to smells. They are often overly sensitive to common environmental lights and sounds which normally do not bother people. Other potential symptoms include nausea and vomiting, which can lead to dehydration if not managed properly.
If you are experiencing any of these symptoms frequently, you must speak with your doctor to make an accurate diagnosis and a treatment plan.
Types of Pain Associated with Intractable Migraines
The pain associated with intractable migraine can vary in intensity and character. It is often described as a pulsating, throbbing or stabbing sensation that can be felt anywhere from the forehead to the neck and shoulders. Some people also report feeling pressure or tightness behind the eyes or in the temples.
Frequency and Duration of Intractable Migraines
Intractable migraines can occur several times a week or even daily, and the intensity and duration of each episode can vary greatly. While most episodes last between 4-72 hours, some people have been known to experience headache flares lasting weeks or months.
Diagnosis and Treatment of Intractable Migraine
Diagnosis
Your doctor may diagnose intractable migraine based on your symptoms and medical history. In some cases, they may also recommend tests such as an MRI or CT scan to rule out any other potential causes of your headaches. Once the diagnosis has been confirmed, treatment can begin.
Physical Exam
Your doctor should conduct a physical exam to look for signs of tension or stress which can exacerbate migraine symptoms. They may also check your eyes, ears, nose and throat to rule out any other potential causes of the headaches. Examining areas such as the occipital nerves in the back of the head and the neurological exam are crucial.
Medical History
Your doctor will also ask about your medical history, including any past or present medications. They may also inquire about any family history of migraines and lifestyle habits such as smoking and drinking.
Imaging Tests
In some cases, your doctor may suggest imaging tests such as an MRI or CT scan to check for any structural abnormalities that could be causing the headaches.
Treatment Options
There are different treatment options that your doctor might prescribe.
Medications
Your doctor may prescribe medications such as triptans, gepants, DHE, ditans, over the counter pain relievers, or anti-nausea drugs to help relieve the symptoms of intractable migraine acute exacerbations.
We often bring patients in for 1-5 days of outpatient IV (intravenous) infusions in our headache center to give a combination of medications including DHE in a “migraine cocktail” to try to break up the headache cycle. This is something to ask your neurologist or headache specialist if they are able to do.
They may also recommend preventative medicines such as daily medicines, gepants (Nurtec, Qulipta), once monthly self-injections (Aimovig, Ajovy, Emgality), once quarterly 30 minute IV Vyepti, Botox, supplements, and neuromodulation devices if you are experiencing frequent episodes.
Lifestyle Changes
Your doctor may suggest lifestyle changes such as stress reduction, relaxation techniques, regular exercise and proper sleep hygiene to help reduce the frequency and intensity of your headaches.
Complimentary Therapies
Alternative treatments can also be used to manage intractable migraine symptoms, including acupuncture, acupressure, massage therapy and biofeedback. However, speaking with your doctor before trying alternative treatments is important.
Coping with Intractable Migraine
Here’s how you can cope with intractable migraines:
Self-Care Strategies
Self-care strategies are important in managing intractable migraine symptoms. This can include taking regular breaks, staying hydrated, avoiding triggers and getting enough sleep.
Support Groups and Counseling
Having a strong support system is also essential when dealing with intractable migraines. This can include family members, friends or even online support groups where you can share your experiences with others. Additionally, counseling or therapy may be beneficial in helping you cope with the symptoms and stress associated with chronic migraines.
Work and School Accommodations
If you have difficulty keeping up with your school or work due to intractable migraines, speak to your doctor about possible accommodations that could help make things easier. This could include flexible hours, limiting environmental migraine trigger exposures, reduced workloads, or additional breaks.
Preventing Intractable Migraines
In some cases, intractable migraines can be prevented.
Identifying Triggers
The first step in preventing intractable migraines is identifying the triggers that may be causing them. This can include environmental factors such as bright lights, loud noises or strong smells, and lifestyle habits such as lack of sleep and stress.
Prevention Strategies
Once you have identified your triggers, developing strategies to avoid them is important. This could include wearing sunglasses outdoors, avoiding certain foods or beverages and maintaining a healthy lifestyle. Additionally, getting enough sleep and managing stress levels is important to prevent intractable migraines.
It is also important to remember that intractable migraines are a chronic condition, and it is important to have patience and seek the help of your doctor to manage them. You can still lead an active and fulfilling life with the right combination of medications, lifestyle changes and therapies.
Prognosis and Outlook
The outlook for intractable migraines varies from person to person. However, with the right treatment plan and lifestyle changes, reducing the frequency and intensity of symptoms is possible. Additionally, support groups and counseling can be beneficial in managing the stress associated with this chronic condition.
Conclusion
Intractable migraine is a chronic condition that can be debilitating and interfere with daily activities. Identifying triggers, developing strategies to avoid them, and self-care practices such as taking regular breaks and getting enough sleep are essential in preventing intractable migraines. Additionally, medications, lifestyle changes and complementary therapies may help manage the symptoms associated with this condition. With the right combination of treatments and lifestyle changes, it is possible to reduce the frequency and intensity of symptoms associated with intractable migraine and lead an active and fulfilling life.
Frequently Asked Questions (FAQs)
Q1: What is intractable migraine?
A: Intractable migraine is a chronic condition characterized by headaches that are difficult to treat, often lasting for more than 72 hours. In addition, there is usually a daily or near daily headache of variable intensity. These types of migraines can be debilitating and interfere with daily activities.
Q2: What are the symptoms of Intractable Migraine?
A: The symptoms of intractable migraine are similar to those of other types of migraines. This can include throbbing pain, nausea, sensitivity to light and sound, and vision disturbances. However, they are more persistent and usually daily or near daily.
Q3: How is intractable migraine diagnosed and treated?
A: A doctor usually diagnoses an intractable migraine based on your medical history and symptoms. Treatment for intractable migraine may involve medications, lifestyle changes, and complementary therapies such as acupuncture or biofeedback. Additionally, self-care strategies, support groups and counseling can be beneficial in managing the stress associated with this chronic condition.
Q4: What are some coping strategies for intractable migraine?
A: Coping strategies for intractable migraine include identifying triggers and developing strategies to avoid them, as well as self-care practices such as taking regular breaks, staying hydrated, and getting enough sleep. Additionally, support groups and counseling can be beneficial in managing the stress associated with this chronic condition.
Q5: Can intractable migraine be prevented?
A: In some cases, intractable migraines can be prevented by identifying triggers and developing strategies to avoid them. There are also many preventive treatments available to help lessen the frequency and severity of headaches. Additionally, it is important to maintain a healthy lifestyle, including getting enough sleep and managing stress levels. This can help reduce the frequency and intensity of symptoms associated with this chronic condition.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.