How To Avoid Caffeine Headaches
Caffeine is a staple in many people’s daily routines, often used to jumpstart the day or as a quick pick-me-up. However, it’s important to understand
Caffeine is a staple in many people’s daily routines, often used to jumpstart the day or as a quick pick-me-up. However, it’s important to understand

Headaches are a common ailment that most people experience at some point in their lives. They can be very scary, caused by anything from a

Understanding migraine triggers is crucial for anyone who suffers from migraines. Identifying what triggers your migraines can often feel like a daunting task, as triggers

Are you one of the millions of people who suffer from migraines? Have you ever considered the impact that your gut health may have on

Do you often find yourself waking up with a headache in the morning? It can be a frustrating and debilitating way to start your day.
Do you experience a pounding headache when you stand up? If so, you may be suffering from a low-pressure headache, or CSF leak headache, one

Have you ever experienced dizziness without the classic throbbing pain of migraine headaches? Can migraines cause dizziness without pain? Is there such a thing as

I see patients stuck in the dark lonely rut of chronic migraine all day every day. Chronic migraine is a miserable headache disorder which causes
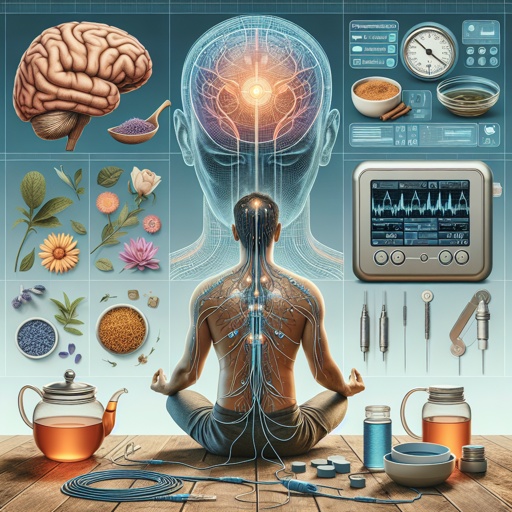
Are you tired of relying on traditional prescription medications to manage your migraine headaches, or do you get every side effect listed on the package

For many people living with fibromyalgia, the battle against chronic body pain is an everyday fight. There is also an intricate relationship between fibromyalgia and