Intravenous DHE (dihydroergotamine) has always been considered to be one of the most effective medicines in treating migraine, refractory migraine and status migrainosus, and cluster headache, when other medicines such as triptans won’t work. DHE is the rare option that can still work when the refractory central sensitization (allodynia) stage of migraine sets in, and it is one of the only options that can reverse this late stage of migraine. This is why it is the staple in IV headache infusions in headache centers.
DHE can uniquely be a 1st line migraine abortive option, in addition to a late stage treatment option (such as status migrainosus). You can see my top 7 reasons and clinical scenarios of when I especially like to use DHE at the end of this article.
So… what if I told you we now have a very easy to use nasal spray DHE with significantly greater effectiveness compared to Migranal and generic nasal spray DHE, with the same potency and effectiveness of IV DHE, but with much less side effects than IV DHE? Well, it’s happened with Trudhesa. And before you start telling yourself this is “just another expensive repackaging of an old medicine that does the same thing”, I have a spoiler alert… that’s far from accurate.
Back in 2009 when I was in my headache fellowship, my mentor and colleague Stewart Tepper MD and I were very excited about a new inhaled DHE being studied called Levadex. So much so that we coauthored this publication about it, and also coauthored a historical perspective and clinical use guidance publication on DHE. Unfortunately, Levadex never came to market. So you can imagine how excited I was when Trudhesa did come to market, also with data showing the same effectiveness of IV DHE without the IV DHE side effects, and without the complicated need to coordinate IV infusions for treatment.
Let me show you the reasons why Trudhesa ain’t your grandma’s nasal spray DHE… but first, we need to discuss a bit of background and perspective on DHE before we get to all the juicy details of Trudhesa…
How Long Has DHE Been Used for Migraine Treatment?
Before we discuss this new refined version of DHE with Trudhesa, it is important to understand the background and history of DHE. DHE is a derivative of the ergots. DHE and the ergots have a rich and fascinating history, including the ergot’s pedigree connection to the hallucinogenic lysergic acid diethylamide (LSD) and the Salem witch trials. But that’s a whole different story… The interesting history and clinical applications of the ergots and DHE can be read in more detail here.
Briefly, ergotamine has been used for a variety of medical purposes since the Middle Ages. In the early 1900s it was approved in the US and had been used commonly as a mainstay of migraine management for many decades.
In 1943, DHE was synthesized as a more potent derivative of ergotamine with lower nausea and vomiting side effects. Unfortunately, unlike ergotamine, oral forms of DHE are not possible due to limitations of absorption and bioavailability. It comes in intravenous (IV), subcutaneous/intramuscular (SC/IM), and nasal spray (NS) treatment options.
The IV form of DHE has always been recognized as the most potent and effective version of DHE in migraine treatment. Unfortunately, it isn’t used as much as it should be given the IV requirement and physician inexperience, making many physicians uncomfortable with its use outside of headache specialists and some neurologists.
The self-injection SC/IM option is second to IV as far as effectiveness. However, this option is somewhat complicated with having to use a filter needle to draw up the DHE in a syringe, then change out the filter needle to a regular needle. Many patients also aren’t comfortable with giving themselves that type of injection or are needle-phobic.
The NS version of DHE debuted with Migranal in 1997, and a generic version became available in 2020. Nasal DHE has always been the “path of least resistance” DHE option, and most patients typically prefer this route vs. IV or a self-injection. However, these historical nasal spray versions (and more specifically, their nasal spray delivery systems) are inefficient. They are complicated to use. The patient has to do a spray in each nostril, wait 15 minutes, then repeat another spray in each nostril. Each spray must be aimed in a very specific way inserted in the nostril, then aimed slightly away from the face to target a vascular area of nasal mucosa. After each spray, the nostril should be held closed for a few seconds. Still, there is often a lot of nasal dripping and a lot of the medicine often goes down the back of the throat as a post-nasal drip, where the DHE will neither be absorbed nor effective.
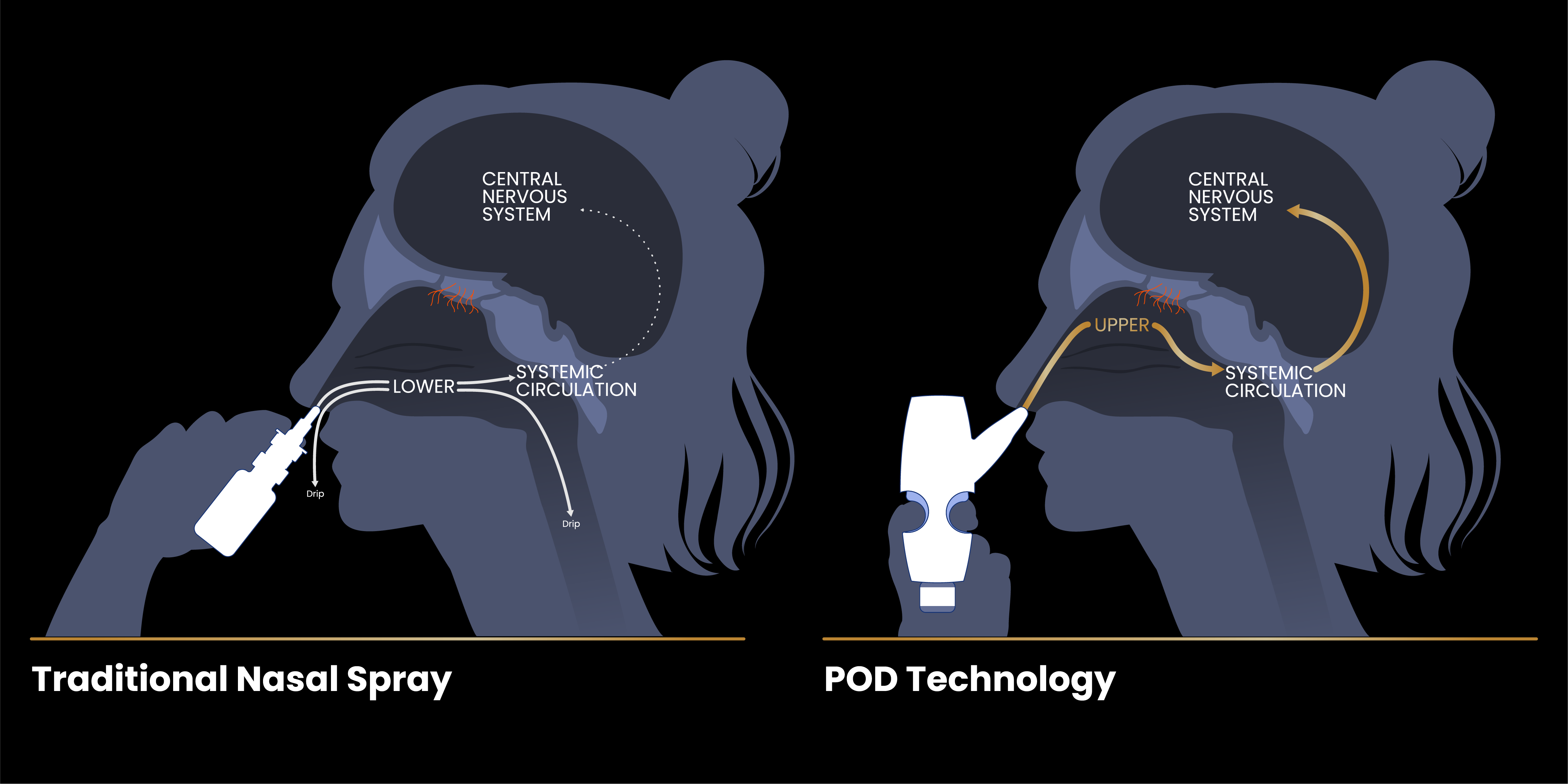
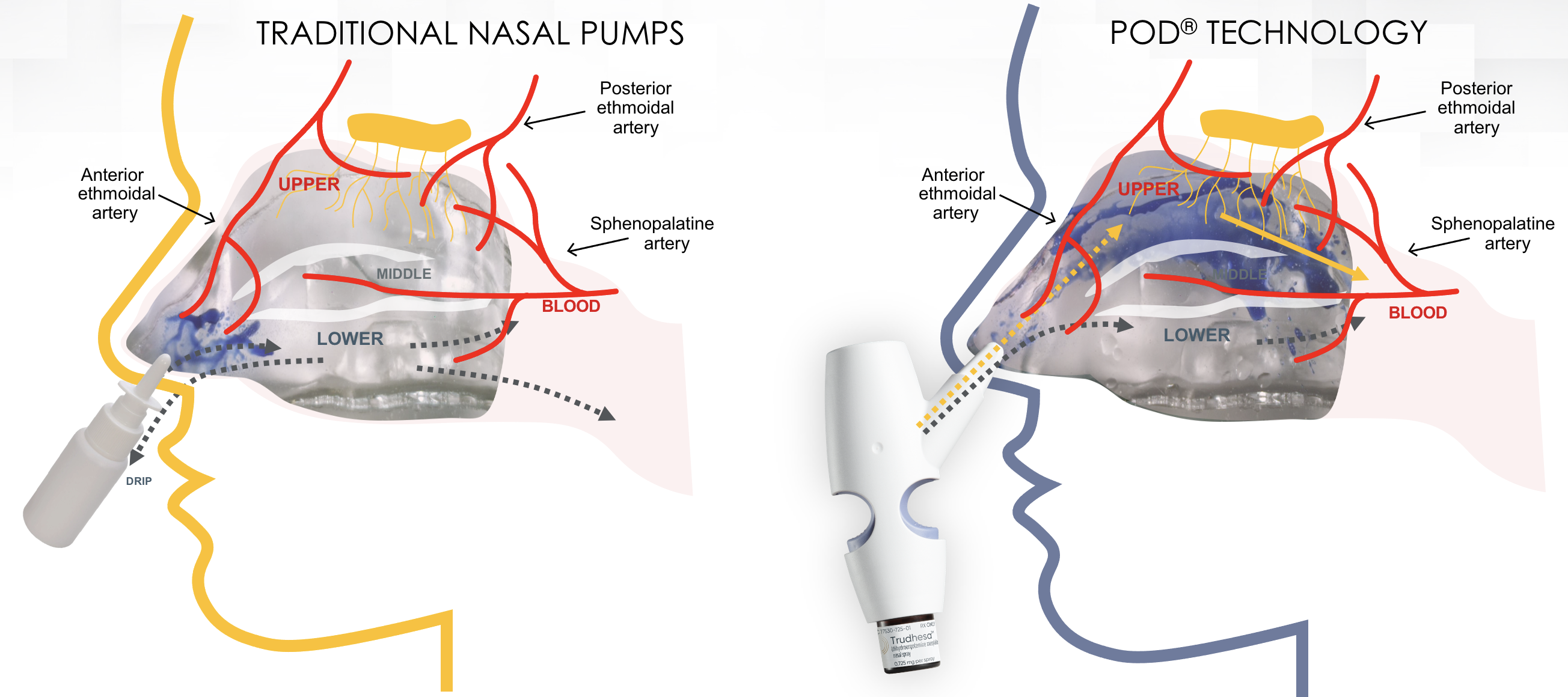
Most recently, a new NS version of DHE was approved in September 2021 called Trudhesa, and it’s a game changer. DHE is DHE and no different than other DHE treatments. In other words, the base medicine DHE is the same. However, the effectiveness of a medicine is dependent on its delivery system. The major difference with Trudhesa compared to prior NS options is in the Precision Olfactory Delivery (POD) technology (see image below). It is this delivery system technology that makes Trudhesa so much more effective compared to older DHE nasal spray devices. And when I say effective, I mean IV level effectiveness minus the IV DHE side effects, as you’ll see below.
How Does DHE Work?
Think of DHE like a mega supercharged triptan +. In fact, the triptans were derived from DHE in terms of their select migraine receptor targets involved in migraine pathophysiology. DHE activates (agonist) the same receptors that triptans activate (serotonin (5-HT) 1B and 1D sub-receptors).
Agonism at 5-HT1B receptors constricts the pain producing intracranial, extracerebral blood vessels in the meninges. 5-HT1B receptors are also present in the brainstem, with unclear significance in relation to migraine.
Agonism at 5-HT1D receptors presynaptically inhibits trigeminal peptide release including CGRP release, and interferes with central trigeminal nucleus caudalis pain transduction and processing, while those of the nucleus tractus solitariuus in the brainstem inhibit nausea and vomiting.
Ultimately, these serotonergic effects result in reversal of vasodilation, decrease in neurogenic inflammation, reduction of central pain signal transmission to the thalamus and cortex, and turn off other ascending pathways to cortex that result in associated migrainous symptoms such as photophobia and phonophobia.
However, and more importantly, DHE also interacts with a multitude of other receptors involved in the migraine circuitry, beyond the triptans receptors. This expansion of receptor interaction besides the triptan receptors is what makes DHE such a powerful migraine option.
We won’t go too in depth in the pharmacology to avoid sending you into a deep sleep with glazed over eyeballs, but to summarize, there are at least 7 classes and 14 subtypes of 5-HT (serotonin) receptors. In general, the 5-HT1 receptors are inhibitory (stopping or “turning off” functions), and the 5-HT2-7 receptors are excitatory (activating functions) in the central nervous system. Ergotamine and DHE also interact with adrenergic and dopaminergic receptors, in addition to a variety of these serotonin receptors, such as 5-HT1A, 1B, 1D, 1F, 2A, 2C, 3, and 4 subtypes. Triptans interact only with 5-HT1B, 1D, and (a few) 1F receptors.
Why Does DHE Work Many Times When Triptans and Other Migraine Abortives Won’t?
The additional migraine receptor targets in addition to the triptan receptors that DHE hits is why it is often helpful when triptans won’t work. For example, about 30% of patients are triptan non-responders. However, many times they may still respond to DHE.
Unlike triptans, DHE can still be effective once the migraine has been continuing past the point of triptans helping. The triptans are made to take at migraine onset, the earlier the better. Once it continues unsuccessfully aborted, it evolves to allodynia and central sensitization. This is the stage of migraine where everything just hurts. For example, people often will say their hair hurts and that they can’t even touch their hair because it is so sore. Triptans won’t touch migraine at this stage, but DHE still can. This is why DHE is usually the most useful medicine used in IV infusions to help break status migrainosus (migraine lasting 3 or more days).
Therefore, another highlight point here is that DHE doesn’t have a true “dosing window” where it has to be taken within a certain time frame for effectiveness, as opposed to all other abortives, as you will further below.
What Are the Side Effects of DHE?
The increased migraine receptor target range is what gives DHE its effectiveness over other abortives. However, the additional targets can also result in increased side effects (particularly for IV formulation). Some of these include agonist activity at 5-HT1A (nausea, dysphoria), 2A (peripheral vasoconstriction), and dopamine D2 (nausea, vomiting) receptors. The 5-HT1B receptors are preferentially expressed in intracranial extracerebral arteries compared with the periphery such as the coronary arteries, where there are more 5-HT2A receptors. Since the triptans are agonists at 5-HT1B receptors, but not at 5-HT2A receptors, they may have less peripheral vasoconstrictive effects compared with the ergots, although coronary vasoconstriction of up to 10-20% still occurs with the triptans according to published evidence.
Who Should Not Use DHE?
Contraindications to DHE use are similar to the triptans. History of coronary, cerebral and peripheral vascular disease, coronary artery vasospasm, pregnancy, breastfeeding, severe renal or hepatic impairment, uncontrolled hypertension, sepsis, following vascular surgery, use of peripheral and central vasoconstrictors, hypersensitivity reactions (particularly to ergot alkaloids), basilar or hemiplegic migraine, and prolonged aura are generally considered the main contraindications.
DHE is also contraindicated within 24 hours of using a triptan, other 5-HT-1 agonists, or ergotamine containing medications.
Can DHE Be Used in Pregnancy or Breastfeeding?
Triptans have historically been suggested to avoid in pregnancy, although classified as category C (some physicians still use them). However, ergots and DHE are classified as category X, because of their history of probable abortifacient effects, and should never be used in pregnancy.
Triptans are often used in breastfeeding now. However, patients should not breastfeed during treatment with DHE, nor for 3 days after the last dose.
What is the Black Box Warning of DHE?
There is a black box warning of peripheral vasoconstriction (narrowing of arteries) when using DHE in combination with potent CYP3A4 inhibitors. There are many common medications that are metabolized by and can influence this liver breakdown pathway. You can discuss with your doctor if you are on any medications that may pose this potential serious or life-threatening interaction. When the CYP3A4 metabolic pathway is inhibited (blocked) by another medication, this can lead to higher blood levels of DHE which in turn can lead to vasospasm causing and ischemia (lack of blood flow) to the brain (stroke), heart (heart attack), extremities (gangrene), and other body tissues and organs.
How Does Trudhesa DHE Nasal Spray Compare to Migranal and Generic DHE Nasal Spray?
First off, there are no head-to-head studies of Trudhesa vs. Migranal nasal spray, Trudhesa vs. generic DHE nasal spray, or Trudhesa vs. IV DHE. The following discussion and data come from comparisons between separate Trudhesa, Migranal, and IV DHE published data and trials. Trudhesa appears to be much more effective than Migranal and generic DHE nasal spray, and this relates purely to its Precision Olfactory Delivery (POD) technology.
The POD technology allows delivery of DHE more strategically and effectively to the vascular rich upper nasal airway. This is in contrast to Migranal which delivers DHE to the lower nasal airway. The obvious difference in drug delivery can be seen in the illustration below.
This is an animation comparing a nasal spray from traditional DHE nasal spray such as Migranal vs. Trudhesa taken from actual spray of each:
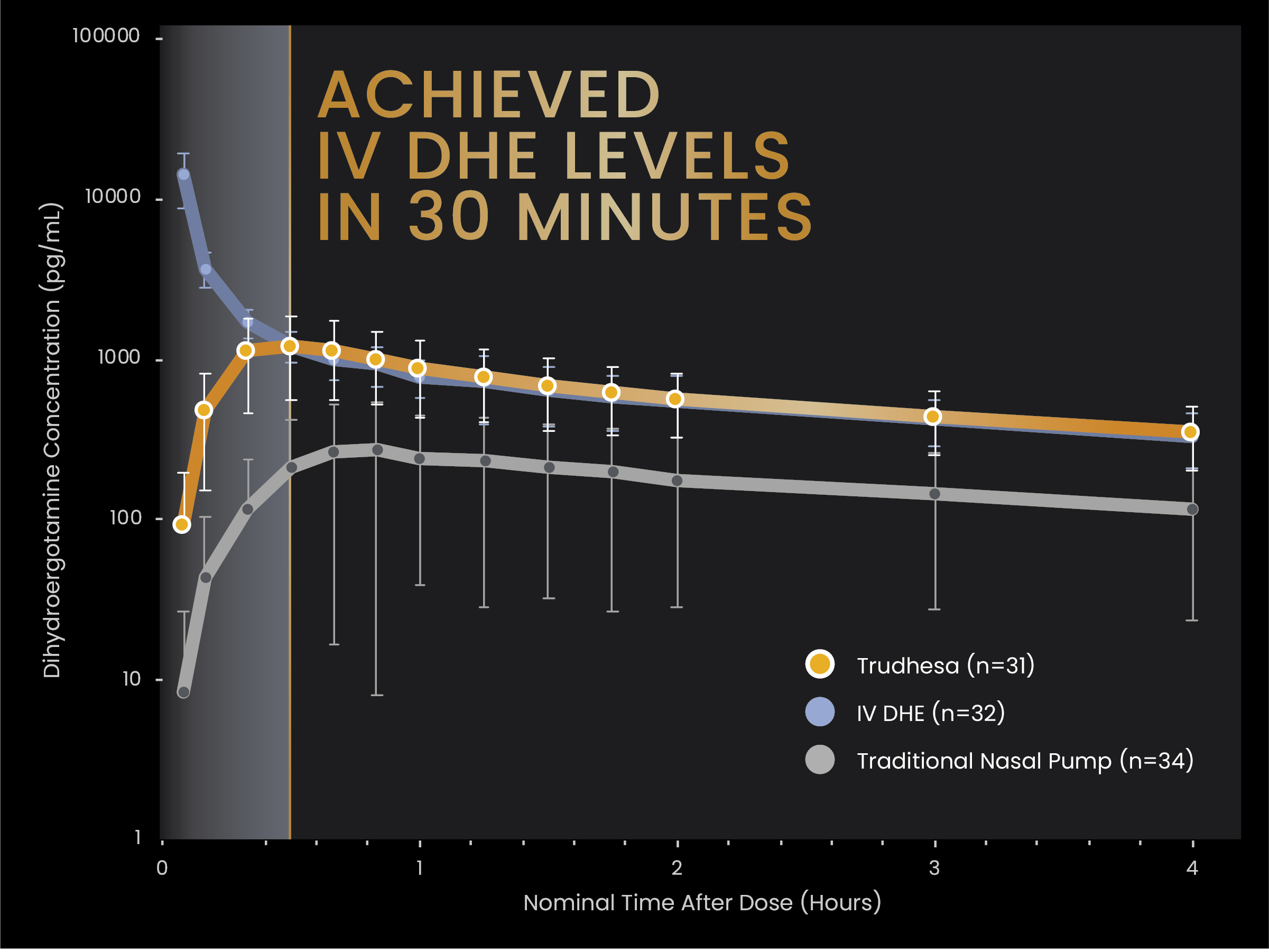
Trudhesa nasal spray has a faster Tmax (time to reach maximum concentration in blood) of 30 minutes compared to Migranal nasal spray at 47 minutes. In other words, it works 17 minutes faster than Migranal.
Trudhesa has 4 times the bioavailability (proportion of drug that enters the blood) than Migranal (59% vs 15%, respectively). What’s really impressive is that this happens despite a lower total dose of DHE in Trudhesa compared to Migranal.
Trudhesa dosing is 1 spray (0.725 mg) into each nostril for a total dose of 2 sprays 1.45 mg. The dosing is very easy to do as seen in this video. Migranal dosing is 1 spray (0.5 mg) in each nostril, then repeat after 15-30 minutes, for a total dose of 4 sprays (2 mg), as detailed earlier above.
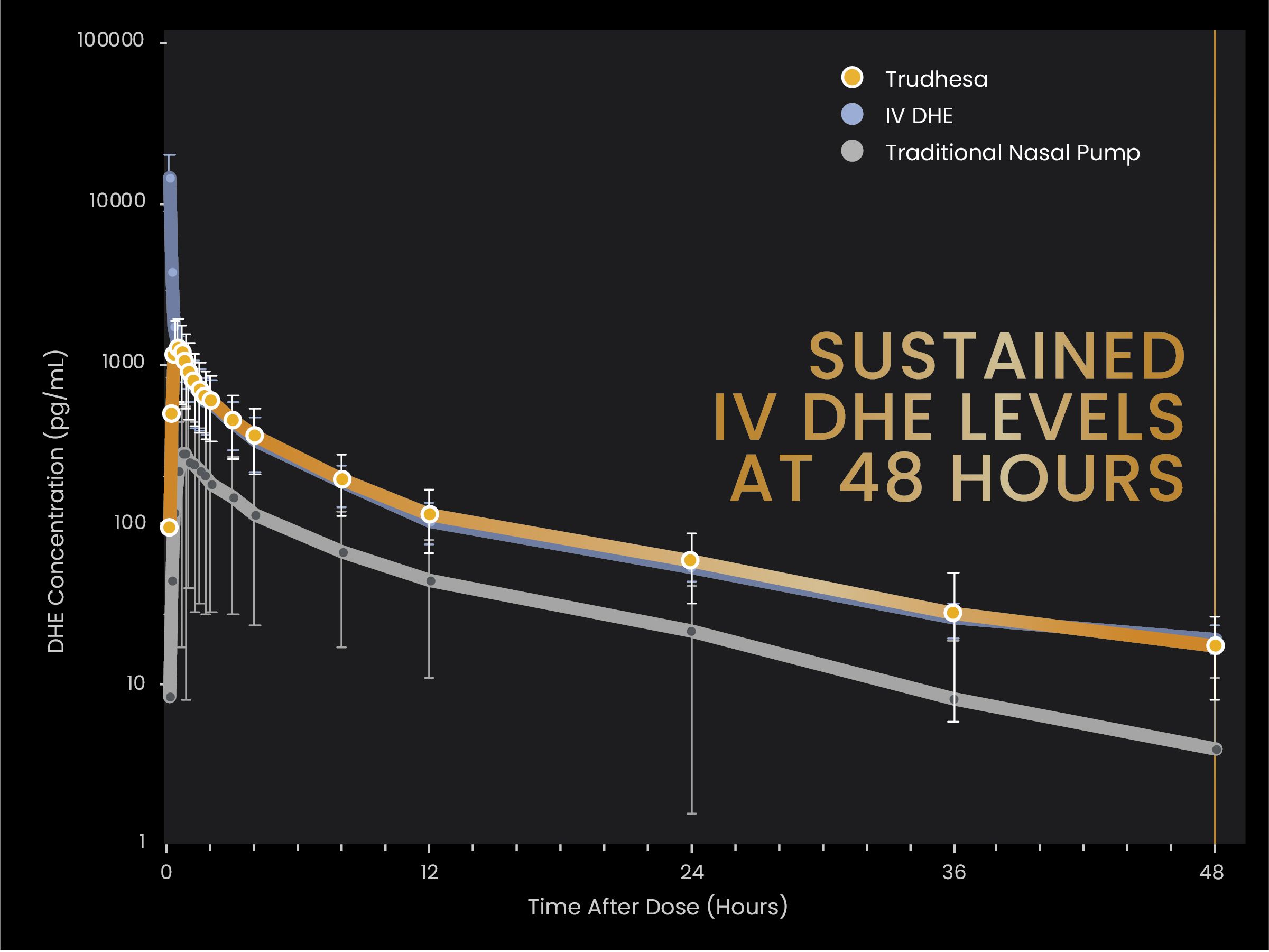
How Does Trudhesa DHE Nasal Spray Compare to IV DHE?
Within 30 minutes Trudhesa nasal spray achieves similar blood concentrations as 1 mg IV DHE, which is quite amazing. Blood levels are sustained essentially the same in Trudhesa and IV DHE through 48 hours. Even more notable is that Trudhesa has a lower Cmax than IV DHE (about 1/10th). In other words, with Trudhesa you do not get that initial Cmax spike that you get with IV DHE. This spike is what causes the common side effects with IV DHE such as nausea and transient increased headache. So in other words, Trudhesa provides almost the same potency, blood concentration, and onset of action as IV DHE, but without the initial medicine spike seen in IV DHE, and thus with much less side effect profile than IV DHE.
Comparisons between all of these data points between Trudhesa, Migranal NS, and IV DHE can be seen clearly in the charts below.
How Effective is Trudhesa?
All of the following efficacy data above are very impressive, especially when compared to the same data end points in the studies of gepants (Nurtec, Ubrelvy), ditans (Reyvow), and triptans (Imitrex, Maxalt, etc.) which can all be cross-referenced in the table here.
Pain Free at 2 Hours
For the 1st migraine attack that Trudhesa was used, 38% of patients were pain free at 2 hours. Of those, 93% continued to be pain free 24 hours later, and 86% were still pain free at 48 hours.
At the end of the study (weeks 21-24), 43% of patients were pain free at 2 hours after taking Trudhesa. Of those, 98% continued to be pain free 24 hours later, and 95% were still pain free at 48 hours!! This highlights the high efficacy and long duration of action of Trudhesa and DHE in general.
Pain Relief at 2 Hours
66.3% of patients had pain relief (migraine moved from a moderate or severe pain level down to a mild or no pain) at 2 hours.
-16.3% had pain relief at 15 minutes
-29.6% had pain relief at 30 minutes
-47.6% had pain relief at 60 minutes
Freedom From Most Bothersome Migraine Symptom at 2 Hours
52% of patients had freedom from their most bothersome migraine symptom (nausea, photophobia, phonophobia) at 2 hours.
Need For Rescue Medication
When Trudhesa was used, 85% of attacks did not require a rescue medication. Again, highlighting the high efficacy and long duration of action of DHE.
No Limiting Dosing Window
Another highlight of Trudhesa and DHE in general is that there is no limiting dosing window. For example, triptans must be taken as early as possible in the migraine attack. The longer someone waits to take a triptan, the less effective it becomes. Trudhesa was just as effective if taken early or if taken more than 4 hours from migraine onset. This characteristic of DHE is why it is generally considered the main ingredient in headache infusions to try to break status migrainosus.
39.3% of patients were pain free in 2 hours if they took Trudhesa 0-2 hours after the migraine began. 39.4% were pain free in 2 hours if they took it 2-4 hours after migraine onset. 30.9% were pain free in 2 hours if they took it more than 4 hours after migraine onset.
Dosing Consistency
An important characteristic of any abortive is that you want it to consistently work. In 65% of patients using Trudhesa, there was a 67-75% consistency that it would give pain relief by 2 hours every time. In 61% of patients, there was a 75-100% consistency that it would give pain relief by 2 hours every time. In 30.4% of patients, there was a 100% consistency that it would give pain relief by 2 hours every time.
What are the side effects of Trudhesa?
The Trudhesa trial (STOP 301) was an open-label pivotal safety study that included 24 weeks of treatment with drug followed by a 28-week extension trial for a total of 52 weeks. DHE has a long track record of clear efficacy (including 4 prior randomized double-blind placebo-controlled trials of nasal spray DHE), so this was not required by the FDA to “prove” efficacy for Trudhesa. We know DHE works. The purpose of the trial was a required safety study given the new POD technology that delivers the DHE, and to observe for other adverse side effects.
6332 doses were administered over the entire 52-week study period. Amazingly, only 0.6% of these doses resulted in nausea. This is really impressive since this has always been the most problematic and reported side effect with all other forms of DHE, especially IV.
Across the 24-week active treatment period, 15% had nasal congestion, 6.8% had nausea, 5.1% had nasal discomfort, and 5.1% had unpleasant taste. There were no clinically significant EKG changes or treatment-emergent adverse events.
Access to Trudhesa
Currently, Trudhesa prescriptions are sent through two specialty pharmacies, either Carepoint Pharmacy (Schaumburg, IL), or Phil (Scottsdale, AZ). They can easily be sent electronically by EMR or by your medical provider filling out and faxing a simple order form to one of these pharmacies. It has been a quick and efficient process thus far from my experience, and the medication is sent directly to your home with a very fast turnaround. Most commercially insured patients have been receiving it for a low $10 copay. It is prescribed with a standard of 8 PODs per month (some insurances allow more). Each POD allows for 1 full dose which is 2 sprays total in the nose (1 spray per each nostril).
My Top 7 Reasons of When to Consider DHE as a Migraine Abortive Over Other Options.
DHE doesn’t necessarily have to be a backup rescue option, and is certainly a perfectly reasonable option as a first line if the patient profile and migraine attack characteristics would be a good fit. However, here are some of the specific scenarios in which DHE can be a very effective option to consider, especially when other abortive treatments have failed to provide adequate benefit.
1. Long Duration Migraines
Migraines of long duration such as menstrual migraine are a good consideration for DHE. DHE has a lower recurrence compared to triptans and many other abortives, so can be very good at targeting this problem.
2. Migraines with High 24-hour Recurrence or Frequent Cluster Headache Attacks
Migraines with high 24-hour recurrence, such as menstrual migraine, that keep returning within 24 hours are a great target for DHE. For example, for many people after the migraine initially goes away with treatment, it continues to come back later in the day or the next day. The end result is that the person ends up with a multiple day migraine. Again, DHE has a lower recurrence compared to triptans and many other abortives, so can be very good at targeting this.
DHE is often helpful in cluster headache as well. Cluster headache attacks can happen multiple times in a day, for which the maximum allowed triptan dosing of twice daily is usually not enough. The long duration of DHE and the ability to re-dose every 8 hours can help with preventing many of the frequent attacks that would otherwise be happening throughout the day or night.
3. Waking Migraines
Waking migraines (you wake with the bad migraine already in process). When this happens, you are typically “behind the ball” of that migraine attack and beyond the stage where triptans will often be helpful. Here is why. Triptans are made to take at the very onset of the migraine and become less effective the longer the migraine goes on. So if you wake with a bad migraine, you are often already past the stage where triptans may be helpful. If you take an abortive pill, you then have to wait for a long time for it to go through the gastrointestinal tract to be absorbed. Or, at that state intractable nausea and vomiting may prevent a pill from even being taken without vomiting it back up. However, DHE can still be effective in the late stages of a migraine, and can be quickly effective since it is a non-oral treatment. This is why it is often used in refractory status migrainosus (a migraine attack lasting more than 3 days) to break a cycle.
4. Moderate to Severe Pain Levels and Presence of Central Sensitization (Allodynia)
If the migraine is in a moderate to severe level of pain (such as when you wake with a bad migraine), including when there is allodynia (central sensitization), DHE is a good option to consider. Allodynia is that later stage of a migraine attack where everything just hurts; your hair hurts and feels sore (some can’t even comb their hair at this stage due to pain), skin hurts, etc. Once you hit this stage, triptans are typically less effective and won’t do much. In contrast, DHE can still be effective in reversing these central sensitization symptoms at late stages of a migraine attack. Again, this is why DHE is often used in refractory status migrainosus to break a cycle.
5. Status Migrainosus Rescue and Cluster Headache
DHE can be used repetitively to break status migrainosus, and can be used repetitively for migraine rescue. I often repeat DHE nasal spray or injections every 8 hours for a few days until a cycle of status migrainosus breaks. It is often also helpful in frequent cluster headache cycles when used the same way.
6. Bridging Out of Medication Overuse Headache (Rebound Headache)
DHE can be used repetitively as a bridge as per #5 above, used to help wean/bridge patients out of medication overuse headache (rebound headache).
7. Fast Onset Nausea and Vomiting
Some patients have very fast onset nausea and vomiting with their migraine. This makes an oral pill abortive worthless because it is just thrown up and isn’t able to get into the system. DHE is a great option to consider for this scenario.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.