Have you lost count of how many migraine preventive treatments you failed? Do you have flashbacks of the terrible side effects that you had to deal with while taking some of those treatments? Have you heard about the migraine surgery, but aren’t sure where to find accurate information on it? Would you like to have the INVENTOR of the migraine surgery answer all your questions? If so, continue reading below…
Over the last several years we have seen monumental steps forward in new migraine abortive and preventive treatments. This seismic shift in new migraine treatment options began when Aimovig (Erenumab) became the first of the CGRP monoclonal antibodies (CGRP mAbs) approved for migraine prevention in 5/2018. This was followed by 3 additional CGRP mAbs; Ajovy (Fremanezumab), Emgality (Galcanezumab), and Vyepti (Eptinezumab).
Following the CGRP mAbs came the gepants for the abortive migraine treatment with Ubrelvy (Ubrogepant) and Nurtec ODT (Rimegepant) in early 2020. Then, the gepants became migraine preventive treatments as well. This occurred first with Nurtec ODT in 5/2021 and then Qulipta (Atogepant) in 9/2021.
Prior to the new migraine preventive classes of the CGRP mAbs and the gepants, there had never been a medicine designed purely for migraine prevention. Prior to these new medications, the main options for migraine prevention included a daily pill from the antiseizure, antidepressant/anxiety and antihypertension (blood pressure) medication categories. Additional migraine preventive treatments have included Botox injections (approved in 2010 for migraine prevention), neuromodulation devices, or alternative treatments such as vitamins and supplements, acupuncture, acupressure and pressure points, or yoga and meditation.
The goal of migraine preventive treatment is to lessen the frequency and/or severity of migraine attacks and are discussed in more detail here. Unfortunately, despite the growing list of available treatment options mentioned above, there are still many patients with heavy and debilitating migraine burden which seems to be resistant to many of these treatment options, or they do not tolerate them. Therefore, they continue seeking other unconventional treatments.
One of those unconventional treatments is what has been referred to as the migraine surgery, and it is performed by only a handful of skilled surgeons.
Given the interest in migraine surgery that many patients ask me about, I have invited one of my colleagues, Bahman, Guyuron MD, FACS, to contribute to this blog article. Dr. Guyuron is the pioneer of the migraine surgery and has an extremely impressive biography as seen at the end of this article, which I recommend that you read through. I have given Dr. Guyuron a list of topics and common questions that patients often have regarding the migraine surgery, and I can think of no one more knowledgeable, qualified, and experienced in this treatment area to answer these questions than the surgeon that invented the procedure himself.
Dr. Guyuron’s pioneering work in the migraine surgery procedure can be further read about at: https://www.drbahmanguyuron.com/procedures/migraine-relief/
Without further delay, I welcome Dr. Guyuron and I thank him for his contribution to this blog article, which I guarantee will be very educational and informative.
The Surgical Treatment of Migraine Headaches
What is the background on the migraine surgery?
Dr. Guyuron discovered migraine surgery in 2000. It began as mere serendipity when patients who had undergone forehead rejuvenation informed Dr. Guyuron that their headaches had ceased. These reports prompted him to activate his research team. Initial investigation of 314 patients who had undergone forehead rejuvenation revealed that 31 of 39 who had migraine headaches had either complete elimination or significant improvement. This encouraging study led to a pilot study involving patients who underwent surgery for treatment of migraine headache and 21 out of 22 patients experienced either complete elimination or a significant improvement of migraine headaches. His research team, including three neurologists, has conducted 44 evidence-based research studies to prove that this surgery not only works, but the results are enduring. Many other centers, including one of the Harvard University plastic surgery research teams, collectively have completed over 50 studies confirming the findings from Dr. Guyuron’s findings.
How does the migraine surgery work?
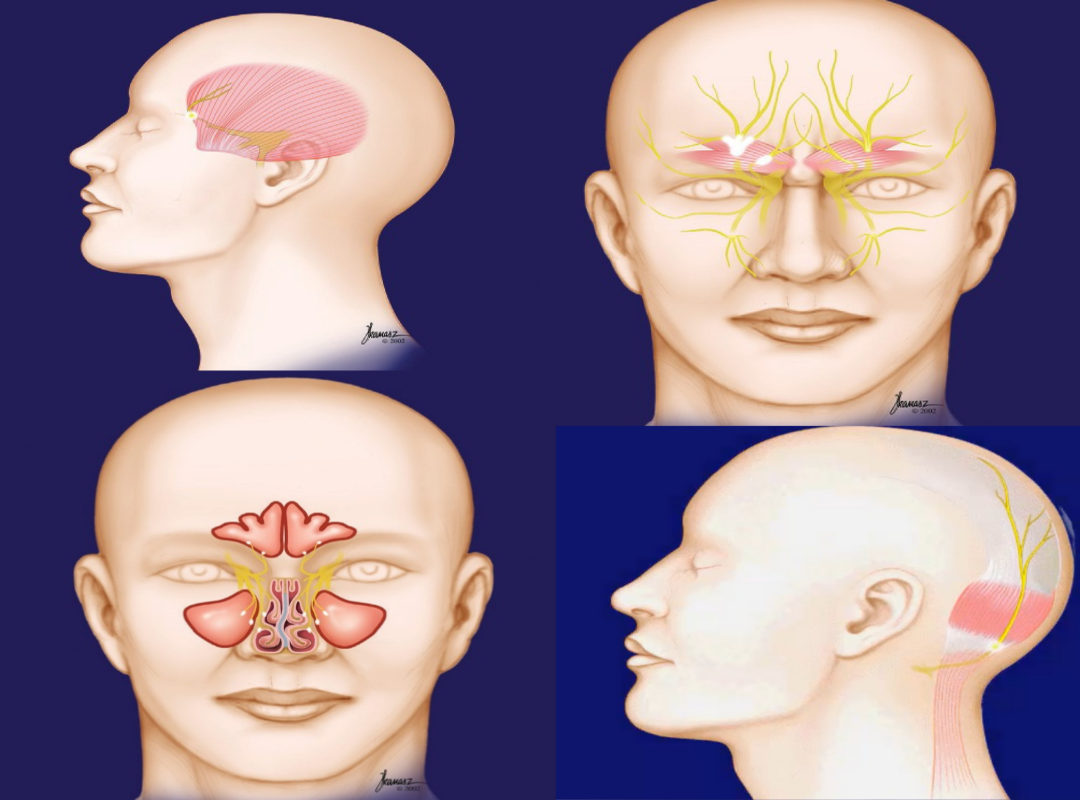
Migraine headaches are triggered by stimulation of terminal end branches of the trigeminal nerve (a nerve that provides sensation to the entire face and head). Dr. Guyuron, through his research and clinical observations, was able to demonstrate that the nerve branches are stimulated by the surrounding structures such as muscles, vessels, bones and cartilage, elimination of which will stop or reduce migraine triggers. Irritation of these branches results in the release of substances that begins a cascade of events, leading to inflammation of the nerves and membranes around the brain that causes symptoms similar to meningitis, thus the migraine headaches. These include nausea, vomiting, and sensitivity to lights and sounds, in addition to the severe headaches. This is why patients usually retreat to a dark and quiet room and try to sleep off this debilitating condition.
Over the years and as a result of the anatomical and clinical research studies, Dr. Guyuron has identified four very common and some uncommon trigger sites. He has developed surgical techniques to deactivate each of these trigger sites and alleviate the migraine headaches. His surgical techniques have been designed to cause the least amount of physiological change locally. In fact, in three sites, the surgery has some side benefits. For example, surgery for migraine headaches in the forehead area involves removal of the frowning muscles (See Video #1 below) which irritate two nerve branches on each side and cause forehead migraine headaches. In addition to stopping the migraine headaches, this surgery results in improvement in the forehead appearance by elimination of the frown lines. In the temple area, the tissues are pulled sideways which results in a gentle lift of the eyebrows and causes rejuvenation of the temples.
Migraine Surgery Video #1: Forehead Area. Video and illustrations provided by Dr. Guyuron.
The surgery in the temple trigger site involves removal of a tiny branch of the trigeminal nerve that provides feeling to this site (See Video #2 below). Detachment of this nerve has been done routinely for other procedures, including surgery around the eye socket or even for cosmetic forehead procedures. Removal of this nerve may often cause temporary or rarely permanent numbness of the temple. Patients do not find the reduced sensation or loss of feeling in this area disturbing since this is not a highly sensitive area. In fact, removal of this nerve, which exits from the site in the temple that most patients commonly rub while having tension or migraine headaches, takes away or reduces migraine and other headaches arising from this area.
Migraine Surgery Video #2: Temple Area. Video and illustrations provided by Dr. Guyuron.
Another trigger site is the septum, the partition inside the nose that divides the interior nose into two spaces. The septum can have a varying degree of deviation. Enlargement of the projections inside the nose, called the turbinates, can be a source of migraine headaches. When there is contact between the turbinates and the deviated portion of the septum or the sharp points within the septum that are called spurs, migraine headaches can trigger (See Video #3 below). After the surgery on the septum and turbinates, which includes straightening the septum and reduction of the size of the turbinates, not only do the patients observe improvement or elimination of the migraine headaches, but they also experience improved breathing (the third example of a side benefit).
Migraine Surgery Video #3: Sinus Areas. Video and illustrations provided by Dr. Guyuron.
The fourth most common site is the back of the head where three nerves can be the source of migraine headaches on each half of the back of the head. The major nerve involved in migraine headaches in this site is called the greater occipital nerve, which is a nerve that originates from the upper portion of the cervical spine (neck). This nerve can be irritated by the surrounding muscles or vessels (See Video #4 below). During the surgery, a small piece of muscle is removed from around the nerve and replaced with fatty tissues from underneath the skin to shield the nerve and separate it from the muscles. The chance of recurring pain will be extremely remote. Additionally, this nerve is decompressed (released) in several sites along its course through the same incision. If the greater occipital nerve is irritated frequently, it can become chronically inflamed. This is called occipital neuralgia. The treatment is essentially the same. A small percentage of patients may have headaches from irritation of another small nerve branch in the upper neck which is called the lesser occipital nerve. Dr. Guyuron has developed a surgical treatment for this site as well. There are other less common trigger sites which include the area above or behind the ear. The pain in this site is eliminated or reduced by removal of a vessel that is compressing and irritating the nerve or by removal of a minor nerve.
Migraine Surgery Video #4: Occipital Area. Video and illustrations provided by Dr. Guyuron.
Where are the incisions for the migraine surgery?
The surgery is done using minimally invasive techniques. For deactivation of the forehead and temple trigger sites in combination, five or six small incisions are made, each approximately one-half inch long. All of the incisions are placed within the hair-bearing skin so that they are not often visible after they heal, as long as the patients heal normally. For isolated forehead migraine headaches, which are extremely rare, the incision can be made in the upper eyelid crease, the incision that is commonly used for cosmetic eyelid surgery. This area heals very favorably on most patients. For the patients with isolated temple headaches, two incisions, each one-half inch long, will be in the temple hair. Surgery in the back of the head is done through an incision about one-and-a-half inches long located in the middle of the scalp right above the neck within the hair-bearing skin. The surgery on the septum and turbinates is done through the nostrils and there are no incisions related to the surgery that can be visible.
What are the risks of the migraine surgery?
Any surgery has potential risks, and this operation is no exception. However, complications are usually minimal and rare. Infection and bleeding may occur, but these are highly unlikely. Every patient will experience some numbness in the surgery site. This is an expected part of the surgery and is not considered a complication. There is a chance that the numbness can be long-lasting or permanent. Rarely, minimal hair loss around the incision can occur. This is often temporary. Another possible, but extremely rare, complication is the development of a neuroma (scarring of the nerve ends) that may cause continuous pain. This may require additional surgery. The nose can become drier after the surgery. If this occurs, it is usually temporary, but in rare cases, this can become permanent. Damage to the nerves that move the muscles may occur, although this is also extremely rare and often temporary. There is a small chance that additional trigger sites may be discovered after deactivating the most prevalent trigger sites. Blood clots can form in the legs and may travel to the lungs, but this is exceedingly rare and it could be life-threatening.
What are the chances of success from the migraine surgery?
Dr. Guyuron’s study results, which have been confirmed by many the studies from many centers, have demonstrated a success rate of between 83-92%, depending on the type of condition and the nature of the surgery. Success is defined as at least a 50% reduction in migraine headache frequency, intensity, or duration. However, more and more, Dr. Guyuron is achieving complete elimination because of his experience in detecting the trigger sites and some refinements in the techniques that he has implemented over the years since he began this surgery.
Where is the migraine surgery performed?
The surgery is usually performed as an outpatient operation in a facility adjacent to Dr. Guyuron’s office.
What type of anesthesia is used for the migraine surgery?
The larger procedures are often done under general anesthesia and usually the patient spends about half a day in the facility. However, many of the patients can undergo the procedure under local anesthesia and return to work the same day or the next day.
What kind of postoperative care is needed for the migraine surgery?
The patient is often discharged home with minimal care required. Someone must stay with the patient the first night to assist the patient in an unlikely emergency, if the surgery is done under anesthesia. There will be a need for application of some ointment on the incisions periodically during the first week. All of the stitches are dissolvable, and they do not need to be removed. After a septum surgery, Dr. Guyuron places two tubes inside the nose, instead of packing, that are not visible from the outside. These tubes will be removed in four to seven days after surgery, depending on the type of surgery.
Who is a candidate for the migraine surgery?
Anyone who has at least two or three severe migraine headaches per month that would not respond to over-the-counter medications, those who are tired of taking migraine medications or not responding to them, and those who experience migraine headaches that interfere with their personal and professional lives would be good candidates for this surgery. This is especially true for those who have frequent migraine headaches, do not tolerate migraine medications, or have experienced side effects from medications.
What kinds of tests are needed for the migraine surgery?
Patients will undergo standard testing as outlined in the anesthesia policy. In addition, for patients who have pain behind the eye, a CT scan may be required to document the abnormalities inside the nose and sinuses which are not easily visualized by simple inspection of the inside of the nose. For those patients who will undergo the surgery with local anesthesia no testing is needed.
What is the recovery like for the migraine surgery?
It all depends on the type of surgery that is needed. After recovering in the facility, if the surgery done under anesthesia, the patient will be transferred home, or to a hotel room close to the surgical facility. When the surgery is done under local anesthesia, the patients will not need recovery time in the facility. The patient may experience some swelling and bruising, when the surgery is to eliminate the forehead headaches, which will get worse within 48 hours and then gradually disappear, on average, in 8-10 days. The patient will appear presentable in about 1-2 weeks after surgery and can resume social activities at this time. The patients undergoing surgery in the other trigger sites, especially for those done under local anesthesia, there is no social recovery. After the extensive surgeries it is recommended that patients avoid heavy exercise for about 3 weeks. Usually there are no limitations after this period. Patients who undergo septum and turbinate surgery, are asked to irrigate the nose once or twice a day for a period of 3-6 weeks.
How does the patient prepare for the migraine surgery?
The patient will be asked to avoid aspirin or aspirin-type medications for 3 weeks before and 1 week after surgery and will be provided with a list of medications and food products to avoid. Strict adherence to the instructions from the surgical team will ensure a safer operation and quicker recovery.
When does the patient notice improvement after the migraine surgery?
Depending on the trigger sites, the results could be experienced the next day or may take several weeks or months to observe the improvement, especially when the surgery involves the nose.
What happens if my migraine headaches do not go away with the migraine surgery?
This commonly is the consequence of the trigger sites that were not identified because they were masked by the more dominant trigger sites. It is always possible to have surgery on the other trigger sites that were not detected earlier. It is extremely rare for the surgery to totally fail. The pain in the operative site may go away completely and you may develop pain somewhere else, which can be treated. Dr. Guyuron always has additional options for all patients, if needed and does not give up easily.
Can I take my migraine medications after the migraine surgery?
If you have migraine headaches, you can continue with your migraine medications, as long as they do not contain aspirin or aspirin type medication. However, the need for these medications becomes extremely small.
Does insurance cover the migraine surgery?
It depends on the type of insurance you have. Approximately 50% of insurance companies currently cover this surgery. Dr. Guyuron’s office staff will assist you in obtaining the answer from the insurance company.
About Dr. Guyuron

Dr. Bahman Guyuron completed a residency in general surgery at Boston University in 1978 and a residency in plastic surgery at The Cleveland Clinic Foundation in 1980. Dr. Guyuron also fulfilled a fellowship in craniofacial surgery at Toronto University Hospital for Sick Children in 1980. He is certified by the American Board of Surgery and the American Board of Plastic Surgery.
Dr. Guyuron has served as Director of the Section of Craniofacial Surgery at the Cleveland Clinic Foundation (1981-1983), Chief of the Division of Plastic Surgery at Mt. Sinai Medical Center (1986-1993). After serving as the Division Chief for 14 months and founding and chairing the Department that he founded for almost 8 years at University Hospital Case Medical Center and Case School of Medicine, he has transitioned to private practice as of January 2015 with full continued commitment to residency education and research, under the title of Emeritus Professor.
Starting his career with a primary focus in craniofacial surgery, Dr. Guyuron has since applied these principles to aesthetic surgery, where he has developed an international reputation for his innovations in rhinoplasty and facial aesthetic surgery. Over the last 21 years, he has captured the attention of the medical and surgical communities with the development of the surgical treatment of migraine headaches with over 44 peer reviewed publications on this topic alone.
Dr. Guyuron has published over 290 articles in peer-reviewed journals, 63 book chapters, and 6 textbooks. He currently serves as Editor in Chief of Aesthetic Plastic Surgery. He served as an Associate Editor of Plastic and Reconstructive Surgery. Additionally, Dr. Guyuron has been intimately involved in the education of plastic surgery through his participation in over 1275 presentations at regional, national, and international conferences. He has lectured in over 30 countries and has served as a Visiting Professor in every respected US medical school. Dr. Guyuron has served in leadership roles in numerous professional organizations in plastic surgery, including the American Board of Plastic Surgery where he served as a director from 2005-2011. He also served as the President of the American Association of Plastic Surgeons, American Society of Maxillofacial Surgeons, Aesthetic Surgery Education and Research Foundation, The Rhinoplasty Society, Northeast Ohio Society for Plastic and Reconstructive Surgeons and Ohio Valley Society for Plastic and Reconstructive Surgeons. He has received numerous awards for his accomplishments from every prestigious plastic surgery organization.
Dr. Guyuron’s pioneering work in the migraine surgery procedure can be further read about at: https://www.drbahmanguyuron.com/procedures/migraine-relief/
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.