Occipital Neuralgia Symptoms, Causes, and Treatments
Occipital Neuralgia Symptoms
What is occipital neuralgia? Occipital neuralgia can be a severe pain and headache in the back of your head and base of your skull, sometimes extending to the top or side of the head or even pain in or around the ear. I tell patients to think of occipital neuralgia like “sciatica of the head”. Similar to that severe pain shooting down the back of the leg in sciatica, occipital neuralgia can be thought of similarly, but the shooting pain goes up into the base of the skull and back of the head. Both of these types of pains are caused by nerve irritation.
Occipital neuralgia first symptoms are often a discomfort in the back of the head and pain at the base of the skull. It can range from sharp and shooting to dull, achy, pressure. Aching pain at base of skull, pain behind ear base of skull area, pain in back of head and in ear are all common areas for occipital neuralgia pain. When pressure is applied to the back of the head (such as during sleep), it often irritates the nerves and flares up the pain.
This back of head pain is typically focused in the suboccipital region (where the base of the skull meets the top of the neck) and occipital region (pain at base of skull and/or back of head). It radiates variably into the back, sides, and top of the head (by the greater occipital nerves) and there is often pain behind the ear on the affected side as well (by the lesser occipital nerves). It can be one sided or both sides.
Symptoms of occipital neuralgia pain are variably described as stabbing, sharp pain, shooting, shocking, or burning pain. It often occurs in attacks of pain which may last seconds to minutes, but can also be a continuous unrelenting chronic pain. Sometimes it may not be as intense and may be a lower-level pain such as pressure, aching, soreness or throbbiness. The back of the skull bone often feels very sore or tender along the bottom of it. The pain and tenderness increases by pushing on the back of the head and along the skull bone base, or lying on the back of the head. This is a good physical examination test at home for occipital neuralgia, and required for diagnosis of occipital neuralgia.
Some patients may have a sensation of numbness or tingling in the back of the head. These headaches and neck pain are commonly intermingled. There may or may not be associated cervicogenic headache (headache coming from the back of the neck) associated with occipital neuralgia. A history of neck injury may accompany this possibility.
Although patients often have isolated occipital neuralgia, I see many patients with occipital neuralgia who also have associated migraine and chronic migraine. This always creates an even more miserable feedback loop between frequent exacerbations of both the occipital neuralgia and migraine headaches. The reason is because these two types of headaches can influence and feed into each other.
For example, 70% of patients with episodic migraine will get neck pain and tightness at the beginning of a migraine attack. So, if someone is stuck in a smoldering cycle of chronic migraine (15-30 days per month), neck pain and occipital neuralgia are commonly associated. The flip side is if someone has structural abnormalities in the cervical spine (herniated disc, injury, whiplash, etc.), it can also be a contributor to frequent or daily headaches.
Occipital Neuralgia Causes
What causes occipital neuralgia? The cause of occipital neuralgia is most commonly idiopathic, meaning there isn’t a specific cause. Another common cause of occipital neuralgia can be from a lot of arthritis in the upper cervical spine (neck), tight muscles through the upper neck and skull base, or following a viral illness which can cause the occipital nerves to become inflamed and irritated.
If you have had surgery or an injury to the back of the head, this can cause scarring of the tissues in the back of the head and base of the skull where the occipital nerves travel. This scarring can pull, twist, and tangle up the occipital nerves over time which causes persistent occipital pain in the back of the head. If the medical history includes whiplash or neck injury, this can also contribute.
Treatment for Occipital Neuralgia
What are the best occipital neuralgia treatments? Neck physical therapy should always be considered as a first line type of occipital neuralgia treatment. The goal is to stretch out and loosen the muscles below the skull base and neck. The occipital nerves pierce directly through these muscles as they travel to the back of the scalp. So imagine what is happening to those nerves if these muscles are in a state of constant tightness and spasm. The muscles will continually squeeze and irritate the nerves traveling through them, which keeps them irritated and keeps the pain going.
Along with the neck physical therapy, I typically suggest a daily preventive medication until the patient is consistently doing much better for several months. A more detailed list of commonly used medications for occipital neuralgia can be read here. In general, typical first line options are the anticonvulsants such as Gabapentin (Neurontin), Pregabalin (Lyrica) or the antidepressant/anxiety class of medications such as the tricyclic antidepressants (Amitriptyline (Elavil), Nortriptyline (Pamelor)) or SNRIs (Duloxetine (Cymbalta) and Venlafaxine XR (Effexor XR)). As needed NSAIDs and muscle relaxants can help with associated muscle spasms.
Additional occipital neuralgia treatment options include occipital nerve blocks (discussed below), occipital nerve stimulation, or occipital nerve decompression, which is a minimally invasive surgical treatment to detangle the occipital nerves through the scalp tissue. Occipital nerve decompression can be very effective at pain relief by releasing the tangled, twisted and irritated occipital nerves as they travel through the fibrous scalp tissue. Occipital nerve decompressions are performed by a few plastic surgeons who are specially trained in this specific procedure. Most centers have moved away from occipital nerve stimulators since insurance rarely covers them, and there are common problems with lead migration (leads move out of place) or lead infection.
If there are associated migraine headaches, a migraine preventive medication or treatment should be chosen, optimally one that can be helpful for both disorders. Botox injections in particular are a great consideration for the combination of chronic migraine and occipital neuralgia because it can be very effective for both. I always give additional dosing over the occipital nerves in this scenario (at least 25 units on each side in the occipital area in the back of the head). A good abortive (as needed) option for migraine attacks, as well as inflammation of the occipital nerves should also be incorporated. Anti-inflammatory medications known as NSAIDs (non-steroidal anti-inflammatory drugs) can be helpful for both migraine and the occipital neuralgia component. Diclofenac potassium tends to be one that I prefer, but some prefer Ibuprofen or Naproxen. If NSAIDs are not effective for aborting the migraine, then a more migraine specific option should be used such as a triptan, gepants, ditans, or a neuromodulation device could also be considered.
If there is a strong cervicogenic component along with the occipital neuralgia, pain management procedures such as cervical facet blocks or cervical epidural injections can also be helpful. However, if the patient has only occipital neuralgia and not much of a neck pain component, cervical facet blocks and other procedures targeting the cervical spine are typically not helpful. If there is a strong neck pain component, sometimes these types of injections can be more helpful at treating not only the neck pain, but also the pain “upstream” since the occipital nerves are branches from the upper cervical spinal nerves.
Occipital Nerve Blocks
Greater occipital nerve blocks and lesser occipital nerve blocks should be considered if the pain is really miserable because these can “cool down” the pain quickly as preventive pain medicines gradually start to take effect. An occipital nerve block is easy to perform in the office, can provide quick relief, and take less than a minute to do. These can act as both an abortive option to break a flare of both migraine and occipital neuralgia. Unfortunately, they are typically more of a temporary benefit (days to weeks to months). Some patients can get 3 months of relief until they wear off. I’ve even seen a few patients receive quick pain relief, and never had return of the pain again, but this occurs much less frequently.
Pain relief typically occurs rapidly, often within minutes of the procedure, and full benefit should be seen by 1-2 days. There may be some associated temporary numbness in the back of the scalp after the blocks. If they are done with steroids, they should not be repeated at intervals any less than 3 months. If they are done without steroids, there is no limitation on how frequent they can be done.
I prefer to have the patient sitting up on the side of the exam table. Some physicians have them sit backwards on a chair, resting their arms and head on the back of the chair. These are done with an anesthetic (numbing) medication such as Bupivacaine, Lidocaine, or Ropivacaine. Some physicians combine these with steroid injections, most commonly Triamcinolone (Kenalog) or Betamethasone (Celestone).
The existing (limited) evidence suggests steroids do not add much value to occipital nerve blocks, unless they are done for cluster headache. However, anecdotally many physicians still feel patients tend to do better with steroids, which makes sense given the inflammatory component of occipital neuralgia and potent anti-inflammatory effect of steroids.
I use a small ½ inch 30-gauge needle (same as for Botox) to minimize the temporary pain of injection, although it takes a bit more force to inject the medicine through the needle. Others use a 28 or 27-gauge needle. I would suggest avoiding anything larger diameter than this since the larger the needle, the more painful the injections are.
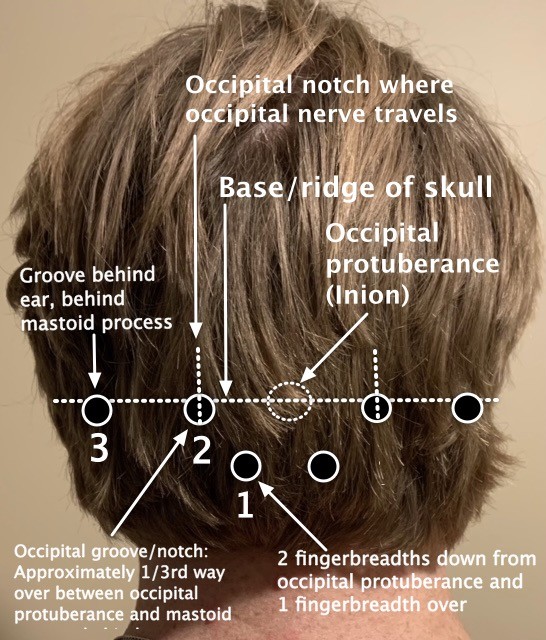
I do 3 injections per side of occipital neuralgia (or both sides if both are affected) to ensure the occipital nerve is treated at all major points. These spots are illustrated on the photograph below. Some physicians do only 1 or 2, so this varies between physicians.
The 1st injection site is located by feeling the occipital protuberance, or inion, (bump in the middle along the skull base), and going 2 fingerbreadths down and 1 over. This is the region where the greater occipital nerve pierces through the musculature.
The 2nd injection site is located just lateral to the occipital protuberance, about 1/3rd of the way over between the occipital protuberance and the mastoid process behind the ear. Feel for a small groove in this area. This is the occipital groove, or notch, where the occipital nerve travels. The patient typically has the most tenderness over this spot as well, so it is typically quite easy to find. The occipital nerve travels along side the occipital artery, so it’s important to withdraw the syringe in this location, as well as all locations, prior to injection to ensure there is no blood retraction into the syringe.
The 3rd injection site is located just behind the ear, posterior to the mastoid bone in another palpable groove. This is where the lesser occipital nerve travels.
Side effects of occipital nerve blocks are typically minimal and well tolerated. There are no limitations to activity afterwards and they will not make you drowsy. Some temporary tenderness in the sites is possible. Dizziness and nausea are infrequent brief side effects. Some patients can develop slight divots in the area of injection if steroids are used. If steroids are used, some patients can also feel more energized for a couple days, and sometimes some flushing.
Occipital Nerve Block Procedure
Here is an example of how I do a typical bilateral (both sides) occipital nerve block procedure (following discussion of risks, benefits, alternatives, informed consent, etc.). If only one side is done, dosing can be split in two.
A combination of Triamcinolone (Kenalog) 40 mg (1 cc) OR Betamethasone (Celestone) 6 mg (1 cc) and 9 cc of 0.25% Bupivacaine was prepared in a single syringe and the injection sites were sterilized with alcohol swabs.
For both sides, the greater occipital nerve was injected 3 cm caudal and 1.5 cm lateral to the inion where the main trunk of the occipital nerve penetrates the semispinalis muscle. The needle was placed perpendicular and the needle advanced 1 cm. After aspiration to ensure no obstruction or presence of blood, the area was injected with 2 cc. The needle was then repositioned at the greater occipital nerve at the level of the occipital groove. After aspiration to ensure no obstruction or presence of blood, the area was injected with 2 cc.
For both sides, the needle was repositioned at the posterior border of the sternocleidomastoid at the level of the angle of the jaw, where the lesser occipital nerve is located. After aspiration to ensure no obstruction or presence of blood, the area was injected with 1 cc.
Conclusions
Occipital neuralgia is a very common but often unrecognized head pain disorder characterized by pain in the back of the head which can range from severe shooting stabbing pain to a dull achy pressure discomfort. For some patients, occipital neuralgia can be a major driver of their chronic migraines. Neck physical therapy and daily preventive medicines that are good for irritated nerve pain are often helpful. Occipital nerve blocks can be performed for quick but usually temporary relief. In more refractory cases for those not responding to these therapies, occipital nerve decompression can also be considered.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.