For many people living with fibromyalgia, the battle against chronic body pain is an everyday fight. There is also an intricate relationship between fibromyalgia and migraines. Both conditions share a common thread of affecting the central nervous system, leading to debilitating symptoms that can greatly impact a person’s quality of life.
Fibromyalgia, migraine, chronic migraine, and irritable bowel syndrome (IBS) are common disorders that tend to cluster together. I tell my patients to think of these disorders as if their central nervous system is in overdrive, overactivated, hypersensitive, and on fire. Think of the central nervous system like a stereo and the volume is turned up full volume with these disorders. Our treatment goals are to find something to help “turn down the volume”.
In this blog post, we will delve into the connection between fibromyalgia and migraines, exploring how these conditions intersect, their correlation with other diseases, and discuss strategies for managing their challenging symptoms.
Understanding Fibromyalgia and Its Broad Spectrum of Symptoms
Fibromyalgia, often misunderstood and misdiagnosed, is a chronic pain condition affecting daily life that manifests as a constellation of symptoms far beyond musculoskeletal pain. If your doctor tells you fibromyalgia is “all in your head”, it’s time to move on to a new doctor who is more up to date with these disorders.
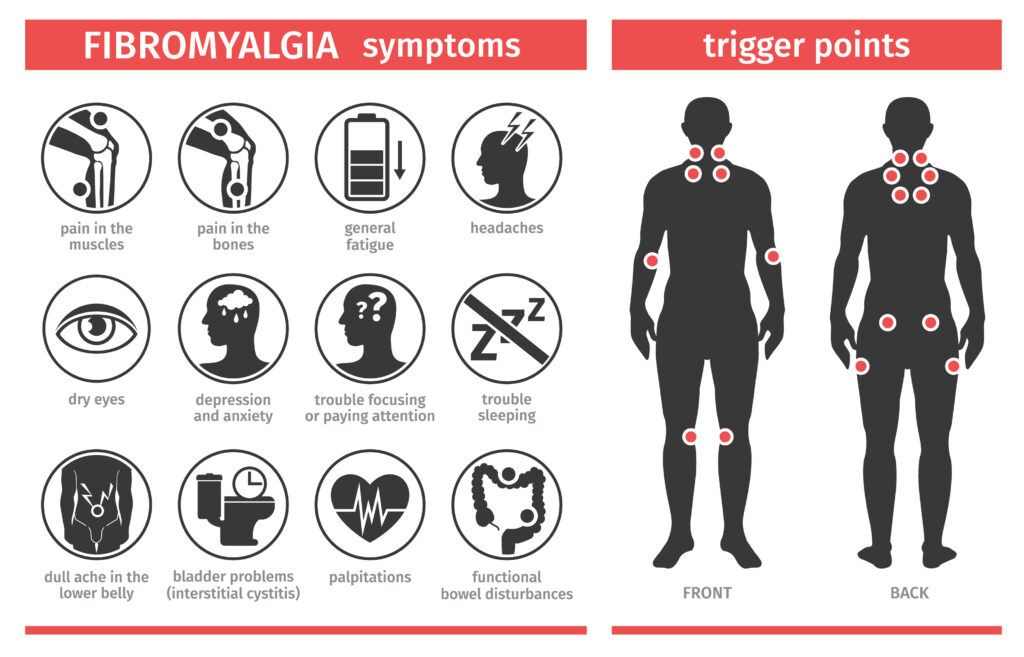
Individuals grappling with this condition navigate a daily landscape filled with challenges, both physical and mental. The hallmark feature of fibromyalgia symptoms is widespread pain throughout the body. There is a wide constellation of fibromyalgia pain descriptions such as muscular aching, burning, cramping, soreness, sharp, and stabbing to name a few.
This chronic body pain is accompanied by a suite of other symptoms that can be just as debilitating. Fatigue, for example, is not just a simple tiredness but a profound exhaustion that doesn’t improve with rest, significantly impacting daily activities and overall well-being.
Since the nervous system is already in a hypersensitive state, constant oversensitivity to stimuli such as lights and sounds is often present, similar to chronic migraine. From my experience, patients with fibromyalgia often tend to be oversensitive to medication side effects as well.
Moreover, fibromyalgia sufferers frequently contend with tender points, specific areas on the body that are painfully sensitive to pressure. Historically, the diagnosis of fibromyalgia was based on diagnostic criteria requiring tenderness or pain in 11 out of 18 specified tender points on the body.
Beyond the physical, the condition often coexists with cognitive difficulties, colloquially known as “fibro fog” or “brain fog”, which can include issues with memory, concentration, and processing speed. Sleep disturbances are also common, with individuals experiencing unrefreshing sleep or difficulty falling and staying asleep, which can exacerbate other symptoms.
Additionally, many with fibromyalgia report mood disorders such as anxiety and depression, further illustrating the condition’s wide-reaching effects on a person’s life. This intricate symptomatology underscores the importance of a holistic approach to care, recognizing the interplay between physical pain and emotional health in fibromyalgia management.
Migraines Unpacked: More Than Just a Headache
Migraines, often misconstrued as “just a headache”, are indeed a multifaceted neurological condition with a symptomatology that extends well beyond head pain. Those afflicted by migraines experience an array of challenging symptoms, including but not limited to, a pulsating or throbbing pain typically on one side of the head (but can be both sides), heightened sensitivity to light and sound, accompanied by nausea, and in some cases, visual disturbances known as aura. These symptoms can be so severe that individuals find themselves completely incapacitated, seeking refuge in dark, quiet rooms to alleviate their discomfort.
The onset of a migraine attack can be triggered by a variety of factors, ranging from hormonal changes, specific foods, stress, and alterations in sleep patterns, to environmental stimuli. This complexity not only exacerbates the difficulty of managing migraines but also underscores the importance of a personalized approach to treatment. It’s essential for migraine patients to identify and avoid their specific triggers, a task that can be daunting but critical for reducing the frequency and severity of attacks.
Understanding the nature of migraines as a neurological disorder sheds light on their unpredictable character and the profound impact they can have on an individual’s life. Migraine and fibromyalgia share many chronic conditions and comorbidities. Recognizing the signs and symptoms of migraines is the first step towards seeking appropriate care and mitigating their disruptive effects. Through a combination of lifestyle adjustments, abortive medication, and possibly preventative strategies, individuals can find relief, though navigating this path often requires patience and perseverance.
Can Fibromyalgia Cause Severe Migraines? The Intriguing Link Between Fibromyalgia and Migraines
The intersection between fibromyalgia and migraine episodes is a topic of growing interest within the medical community, sparking research aimed at unraveling the complex relationship between these two conditions. Studies have increasingly indicated that those living with fibromyalgia are at a heightened risk of experiencing severe migraine attacks, or “fibro migraines”. The link suggests an underlying commonality in the way the central nervous system processes pain and sensory information, pointing to a possible shared pathophysiology.
This heightened susceptibility to migraines among fibromyalgia patients may be rooted in the central sensitization observed in fibromyalgia, where the nervous system goes into a state of high alert, amplifying pain signals. Interestingly, for some people their fibromyalgia begins with a traumatic emotional event and their nervous system seems to “get stuck” in this heightened state. This overactive pain processing could similarly influence the occurrence and severity of migraine attacks, making them more frequent or intense for individuals with fibromyalgia.
Central sensitization, or allodynia, is also a common feature of migraines. This is where the hair and scalp become very sore and sensitive to touch. In fibromyalgia, people often feel this oversensitivity to touch and pain throughout not only the head, but the entire body. Some people with only migraine also describe “full body migraines” where their head and entire body hurt during a migraine. This is almost like a temporary glimpse into the related world of fibromyalgia.
While the precise cause-and-effect relationship remains to be fully elucidated, the co-occurrence of fibromyalgia and migraines underlines the importance of an integrated treatment strategy. For healthcare providers, recognizing the potential for overlapping conditions means a more vigilant assessment of headache complaints in fibromyalgia patients, ensuring that both conditions are managed effectively.
In delving into the intricacies of how fibromyalgia may lead to an increased incidence of severe migraines, it is clear that both conditions share a common link through the central nervous system. Unpacking this connection further could pave the way for innovative approaches to treatment and management, offering hope for those caught in the crossfire of these intersecting conditions.
What Kind of Headaches Do People with Fibromyalgia Have?
Individuals with fibromyalgia frequently find themselves grappling with an array of fibromyalgia headaches, which can significantly contribute to the complexity of their condition. Among these, tension headaches and migraine headaches are the most common types of headaches, serving as yet another layer of discomfort atop the already challenging symptoms of fibromyalgia. These headaches tend to be chronic headaches, meaning they occur on 15-30 days per month. Fibromyalgia and headaches occur together for the vast majority of fibro patients.
Tension headaches, characterized by a persistent dull ache on both sides of the head, often mimic the widespread pain experienced elsewhere in the body by those with fibromyalgia. Migraines, on the other hand, bring a more intense level of pain that can be debilitating, often accompanied by sensitivity to light and sound, nausea, and sometimes visual disturbances known as aura.
The occurrence of these headaches is not merely incidental but is deeply intertwined with the overarching dysfunction of the central nervous system seen in fibromyalgia. This connection underlines the importance of recognizing headache patterns as an integral component of managing fibromyalgia effectively.
By acknowledging the frequency and severity of these headaches, healthcare providers can tailor their approach, offering treatments that not only address the broader symptoms of fibromyalgia but also mitigate the specific challenges posed by tension headaches and migraines. This nuanced understanding is crucial for crafting a comprehensive care plan that seeks to alleviate the multifaceted pain experienced by individuals living with fibromyalgia.
What Diseases are Linked to Fibromyalgia?
Exploring the complex landscape of fibromyalgia reveals an intriguing connection with several other conditions, highlighting the multifaceted nature of this chronic pain syndrome. Notably, fibromyalgia is frequently found in tandem with irritable bowel syndrome (IBS), a disorder characterized by abdominal pain and changes in bowel habits, underscoring a shared sensitivity to pain and discomfort. Chronic fatigue syndrome (CFS), another condition closely aligned with fibromyalgia, mirrors its debilitating fatigue and unrefreshing sleep, pointing towards a common underlying dysfunction in the way the body perceives and manages energy and pain. Ehlers Danlos Syndrome (EDS) can also cause a fibromyalgia-like chronic musculoskeletal pain pattern.
Moreover, individuals with fibromyalgia often find themselves confronting symptoms of various autoimmune disorders, such as rheumatoid arthritis and lupus, which involve the body’s immune system mistakenly attacking its own tissues, causing inflammation, pain, and fatigue. Inflammation of the nervous system from a variety of different causes is suspected to be a primary cause of fibromyalgia.
For some, their onset of fibromyalgia syndrome began after a nonspecific viral illness, suggesting a chronic post-viral syndrome manifesting as fibromyalgia from an ongoing overextended immune/inflammatory response. This is also very common in Long Covid Syndrome, or chronic post-Covid syndrome. This overlap with autoimmune disease for some may suggest a systemic inclination towards heightened inflammatory responses, further complicating the pain management puzzle in fibromyalgia.
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is an illness characterized by disabling fatigue, whereas fibromyalgia is an illness characterized by generalized body pain. However, widespread musculoskeletal pain in response to physical activity is also common in ME/CFS. These disorders often all overlap sharing similar symptoms. Some feel they could simply all be the same disease at different severity levels of the same spectrum.
Additionally, fibromyalgia’s association with mood disorders, including anxiety and depression, reflects the significant psychological burden of living with chronic pain. The intertwined nature of pain and mood in fibromyalgia underscores the need for a holistic treatment approach that addresses not only the physical but also the emotional dimensions of the condition.
This complex web of associations between fibromyalgia and other diseases emphasizes the importance of comprehensive care and the necessity of understanding the broader health context of each individual living with fibromyalgia.
Strategies for Managing Fibromyalgia and Migraine Symptoms
Navigating the turbulent waters of fibromyalgia and migraine symptoms demands a comprehensive, patient-centric strategy that emphasizes not only medical interventions but also lifestyle changes. Key to this approach is the cultivation of stress-reduction techniques, such as mindfulness meditation, yoga, or gentle exercise routines, which have been shown to alleviate the intensity and frequency of both migraine attacks and fibromyalgia flares. Diet also plays a crucial role, as certain foods may trigger symptoms in susceptible individuals; maintaining a food diary can help identify and avoid these triggers.
In addition to these lifestyle modifications, medication therapy should be carefully considered under the guidance of healthcare professionals in the treatment of fibromyalgia. Many of these medicines are also used for migraine prevention as well. These may include pain relievers, specific antiseizure medications such as Gabapentin and Pregabalin known for their pain-managing properties, and antidepressants such as Duloxetine, Milnacipran, and Venlafaxine, which can help manage pain and fatigue associated with fibromyalgia. Ensuring treatment of depression and anxiety that usually come with fibromyalgia is important. Many of these medicines also serve this purpose, and cognitive behavioral therapy can also be a useful addition.
It’s also essential to establish a regular sleep pattern and avoid poor sleep, as quality sleep can help mitigate symptoms of both conditions. Deep sleep stages are where the brain replenishes its neurotransmitters. So if good deep sleep is not obtained, this will only pour gas on the fire and make everything worse. Amitriptyline and Nortriptyline can also help with sleep, as well as pain.
Collaborative care is vital, involving physical therapists, rheumatologists, neurologists, and mental health professionals, to provide a multi-faceted support system. This holistic approach ensures that treatment plans are as dynamic and multifaceted as the symptoms of fibromyalgia and migraines themselves, offering a path towards relief and improved quality of life.
When to Seek Professional Help for Fibromyalgia and Migraines
Navigating the complexities of fibromyalgia and migraines often requires more than self-care and online research. Any type of headache, including migraine, should always be evaluated by your doctor, and include a physical exam. Similarly, any body or muscular pain should also be evaluated by your doctor to exclude other treatable disorders such as a myopathy (inflammation of the muscles).
If your journey through managing symptoms feels increasingly overwhelming, or if you notice a significant change in the pattern, frequency, or intensity of your symptoms, it’s essential to consult a healthcare provider. Whether it’s the emergence of new symptoms or the ineffectiveness of current management strategies, professional guidance can offer critical insights and advanced treatment options tailored to your specific condition.
Understanding the deep-rooted connection between fibromyalgia and migraines illuminates the significant role the central nervous system plays in these conditions. This recognition paves the way for individuals to adopt strategies that target both ailments, aiming for a balanced approach to symptom management. Embracing a comprehensive care model is crucial, one that integrates physical interventions with emotional support, underscoring the inseparable link between mind and body in dealing with these complex disorders.
Healthcare providers are equipped to conduct a comprehensive evaluation, considering the multifaceted nature of these conditions to recommend the most effective course of action. Early intervention can be key in preventing the progression of symptoms and enhancing your quality of life. Remember, reaching out for professional help is a step forward in your path to managing the complexities of fibromyalgia and migraines, ensuring you receive the support and care necessary to navigate these conditions effectively.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.