Optical migraine
Have you ever experienced strange visual disturbances in your field of vision that come out of nowhere? You might be experiencing an optical migraine, also called ocular migraine, ophthalmic migraine, visual migraine, optic migraine, or retinal migraine (the most accurate term). These terms are used interchangeably for this type of migraine. An ocular migraine is a rare form of migraine attack. Unlike classical migraine aura which effects both eyes since it is comes from the brain, optical migraine characteristically only affects one eye since it comes from the retinal nerve layer on the back of the eye. Similar to classic migraine aura, symptoms can include flashing lights, temporary vision loss, and scintillating scotomas. These episodes can be frightening and confusing, but understanding what causes them and how to manage them can help alleviate some of the anxiety they may cause. In this blog post, we will delve into the world of optical migraines to shed some light on this puzzling migraine phenomenon.
What are the symptoms of optical migraines?
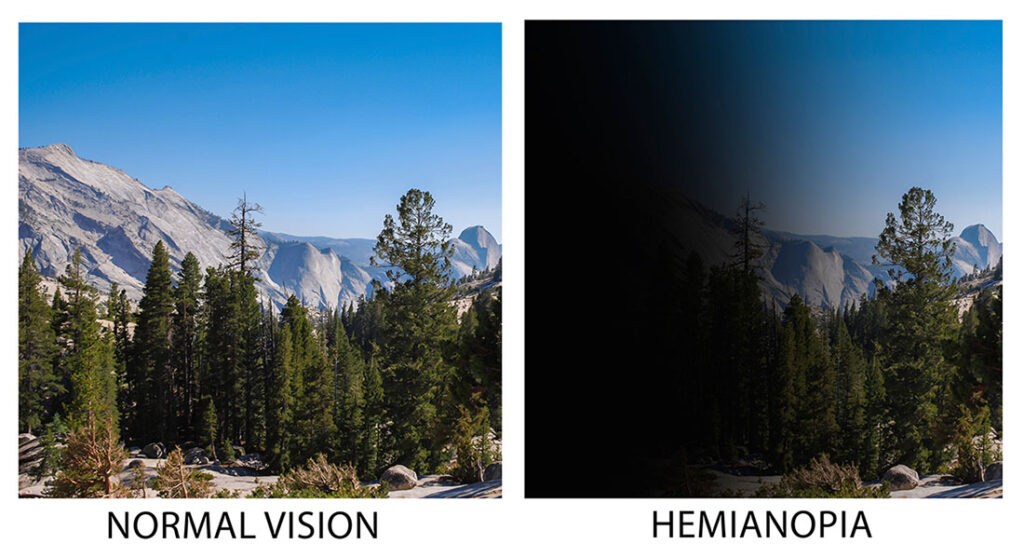
Optical migraines manifest as distinct visual changes that temporarily impact one’s sight. Individuals may notice unusual temporary phenomena such as flashes of light, zig-zag lines, shapes, colors, changes in color perception, jagged broken glass appearances, kaleidoscopes, sparkling or shimmering lights, scintillations, temporary blindness such as hemianopia, or blind spots (scotomata) within their field of vision. These visuals may drift across the eyesight area, often spreading from the outside (peripheral) visual field and moving towards the center. These symptoms are usually brief, lasting 5 to 60 minutes, and occur as a warning sign before the migraine headache starts. However, they may also occur without any headache following (acephalgic migraine). These visual symptoms are isolated to only one eye. So if you open and close each eye individually, one eye will look normal and the other eye will manifest the visual disturbance. This is the key differentiation from aura associated with classic migraines, which occurs in both eyes.

Optical migraine causes. Are ocular migraines in the eye or brain?
Optical migraines originate in the retina of the eye, which is made up of a layer of nerve cells. The phenomena experienced during an optical migraine episode are from transient electrical discharges within that retinal nerve layer. This is in contrast to classical migraine aura which occurs in the brain and is related to changes in blood flow and electrical patterns (cortical spreading depression) occurring in the occipital (visual) cortex of the brain. One theory of ocular migraine is that it is due to vasospasm (temporary narrowing) of the small blood vessels supplying the retinal layer which trigger the symptoms. Another theory is that it is a spreading depression of the retinal neurons in the back of the eye, similar to the spreading depression of the cerebral cortex during a normal migraine aura.
What is cortical spreading depression?
Let me give a quick refresher on what cortical spreading depression is since I’ve mentioned it a couple times. Migraine aura is caused by an electrical wave spreading across the cortex (outside layer) of the brain moving at about 3 mm per minute. At the front of this spreading electrical wave it causes over-activation of neurons and an increase in blood flow. This hypermetabolism causes the “positive” migraine aura features (colors, flashing lights, kaleidoscope, scintillations, zig-zags, etc.). Following this electrical wave there is “neuronal spreading depression” and hypometabolism, associated with a decrease in blood flow. This hypometabolism causes the “negative” migraine aura features (loss of vision, black spots, scotomata, etc.) because the neurons are now temporarily inactive and dysfunctional.
Is ocular migraine a mini stroke?
The similarities between the symptoms of an optical migraine and those of a mini-stroke, or transient ischemic attack (TIA), can be disconcerting. Both conditions may manifest through sudden visual disturbances and can understandably cause alarm. However, it’s crucial to differentiate between the two. Optical migraines and TIAs can both be characterized by temporary visual phenomena without causing permanent brain damage. The underlying mechanisms differ significantly; a mini-stroke involves a temporary block in the blood supply to part of the brain, leading to potential, albeit short-lived, neurological dysfunction. In contrast, optical migraines result from transient changes in the brain that do not impede blood flow to such a critical extent and are from an electrical dysfunction. Prompt medical evaluation is essential for any sudden or severe symptoms to rule out a serious condition and ensure appropriate management. Cases of permanent visual loss associated with retinal migraine have been reported. Other causes of transient monocular (one eye) blindness should always be evaluated for, such as retinal detachment or amaurosis fugax from temporary blockage of blood flow to the retina and eye (a form of TIA).
How do you treat an ocular migraine?
Dealing with optical migraines can be challenging, primarily because there isn’t a one-size-fits-all treatment. Like regular migraine headaches, managing optical migraines requires a personalized approach, emphasizing lifestyle changes, avoiding common triggers and risk factors, and medical interventions. For those with frequent or debilitating episodes, prevention strategies with a doctor becomes essential. This may involve the prescription of medications traditionally used in migraine management, such as beta-blockers, calcium channel blockers, anti-seizure ,or antidepressant medications tailored to reduce the frequency or severity of the migraines. Magnesium and vitamin B2 (riboflavin) can be helpful supplements in lessening visual aura symptoms.
Strategies such as pinpointing and avoiding common migraine triggers play a pivotal role in reducing the frequency and intensity of these episodes. Engaging in regular, restorative sleep, maintaining hydration, and implementing stress-reduction techniques can also make a significant difference in managing this condition. The use of a headache diary can be instrumental in identifying triggers and patterns, providing valuable insights for both you and your healthcare provider. Such proactive measures, coupled with a collaborative healthcare partnership, empower individuals to navigate the complexities of optical migraines more effectively, enhancing quality of life despite this challenging condition.
What vitamin deficiency causes ocular migraines?
Navigating the intricate landscape of optical migraines reveals intriguing connections between nutrition and our neurological health. Some research has suggested that deficiencies in certain vitamins, such as vitamin B2 (riboflavin), vitamin D, or magnesium may have a role in precipitating the occurrence of optical migraines (and any form of migraine). Vitamin B12 can also rarely cause visual symptoms, so should also be checked. Your doctor can offer guidance on appropriate testing for vitamin deficiencies and recommend safe, effective strategies for supplementation.
When to seek professional help for optical migraine
It’s essential to recognize the signals that necessitate medical intervention before assuming symptoms represent one of the many types of migraine. Certain symptoms demand immediate attention: new or intensifying headaches, visual aura symptoms that last longer than 60 minutes, or episodes paired with additional neurological signs like confusion, muscle weakness, or speech difficulties. These could indicate a more serious underlying condition, differentiating them from the typical manifestations of optical migraines. Any vision loss episodes or visual disturbances should always be evaluated by an eye doctor, as well as neurologist. The first time an optical migraine occurs always mandates an evaluation. It’s always better to be on the safe side and get any visual symptoms evaluated. Reaching out to a healthcare professional offers not just peace of mind but ensures that any potentially serious conditions are promptly and appropriately addressed, safeguarding your health and well-being.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.