Long Covid, post-Covid syndrome, long Covid syndrome, long Covid-19, post Covid-19 syndrome, long haul Covid, and long tail Covid are some of the emerging terms for what appears to be a chronic constellation of symptoms following Covid-19 infection in some patients.
What are long Covid symptoms, and what is long Covid syndrome?
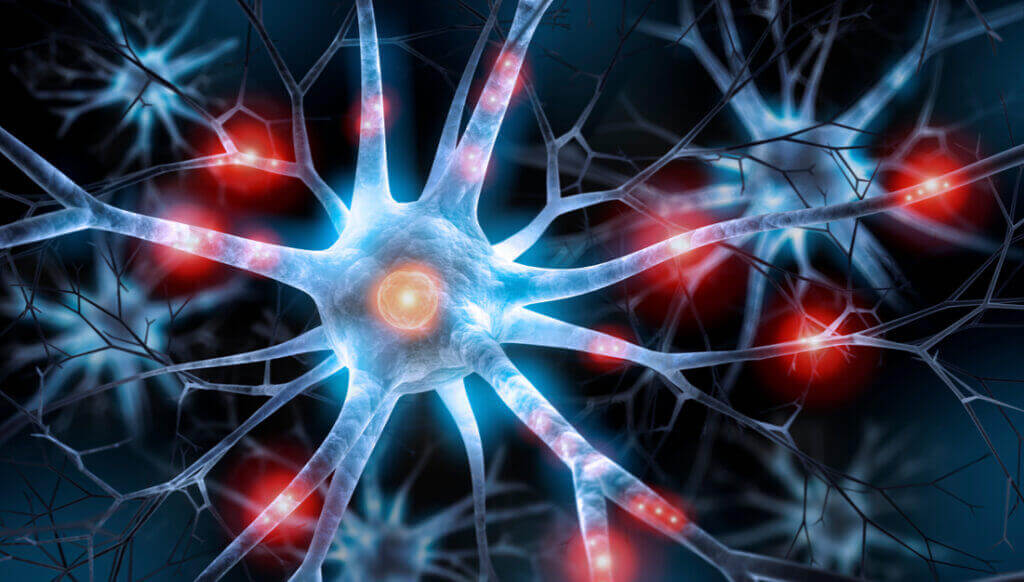
Here is how I want you to visualize long Covid syndrome, or any chronic post-viral syndrome. Close your eyes and imagine your body in its usual shape and form, but with no tissue or anything else except for its vast nervous system and network of nerves throughout every fraction of a millimeter of your body. Imagine this extensive network of nerves as if they are bare metal electrical wires plugged into their source of electricity, the brain, which normally regulates all of these various electrical circuits in the body. Now imagine a bucket of water dumped onto this vast connection of live electrical wires. This immediately causes short circuiting of the electricity running through the nerves, along with smoke, and a smoldering, crackling, buzzing, electrical fire (hopefully you’re getting a good visual there). This is how you can think of post-Covid syndrome, except it isn’t a bucket of water dumped onto the body’s electrical connections, but rather Covid-19 with the same end results of a nervous system meltdown, and often to a much greater degree than a typical case of chronic post-viral syndrome.
So essentially, think of long Covid syndrome as having gotten stuck in an extensive variety of short circuits and nervous system dysregulation because the normal regulating circuits from the brain have been injured and disrupted. The resulting long Covid symptoms are widely variable but most often include headaches, excess fatigue, exercise intolerance, shortness of breath, muscle pains, chest pain, breathlessness, muscle weakness, dizziness, imbalance, disequilibrium, tremors, cognitive fog, tinnitus, brain fog, cognitive dysfunction of memory, concentration, and attention, sleep disturbances, dysautonomia, POTS, dizziness or passing out when standing (orthostatic intolerance), temperature dysregulation, tachycardia (racing heart) with mild activity, night sweats, persistent low grade fever, depression, anxiety, gastroparesis (the gut not transporting food through the digestive tract as efficiently), and other gastrointestinal symptoms such as diarrhea and constipation. These are just a few of the reported chronic symptoms. This study of 3762 patients identified 203 symptoms of long Covid syndrome.
Now keep in mind, this scenario is not specific for only Covid-19. This is a syndrome well known by neurologists and seen not too uncommonly, normally called a chronic post-viral syndrome. Awareness has just become higher given the Covid-19 pandemic and amount of people infected with resultant chronic post-viral syndrome. It usually begins around the time of a nonspecific mild viral illness which you wouldn’t expect to cause any significant complications such as an upper respiratory infection, diarrheal illness, or a vague flu-like illness. Covid-19 is another virus which can also trigger this same syndrome, just as many other viruses have done historically for centuries. However, the chronic symptoms seem to often be much more severe and debilitating compared to other chronic post-viral syndromes.
Many of the long Covid symptoms and other chronic post-viral syndromes have symptoms which overlap with myalgic encephalomyelitis chronic fatigue syndrome (MECFS). Another term for patients with these symptoms is people with myalgic encephalomyelitis (PWME) which is commonly seen discussed on social media outlets. Patients with these disorders often report some nonspecific viral symptoms such as the common cold, runny nose, cough, or diarrhea preceding the onset of their MECFS symptoms. So, a similar mechanism causing MECFS, long-Covid syndrome, and other chronic post-viral syndromes is suspected. Many of these syndromes are also consistent with fibromyalgia syndrome, which shares many similar characteristics. All of these terms should be considered a diagnosis of exclusion, meaning other possible causes should be excluded first. Comprehensive evaluations should include cardiac (heart), pulmonary (lung), autoimmune and rheumatologic (such as lupus, multiple sclerosis, etc.), neurocognitive, sleep medicine, physical therapy, ongoing infections, medication side effects, or other metabolic disturbances depending on what constellation of symptoms the patient is dealing with.
What Causes long Covid syndrome?
Generally, the cause of post-Covid syndrome, similar to other chronic post-viral syndromes, has been suspected to have an immune reaction as the underlying cause of it. The way it works is that your immune system first develops antibodies against a piece of the virus which it encounters, typically a protein. Well, that piece of the virus that your immune system forms antibodies to are meant to attack and neutralize any viruses that enter your body with a similar protein so you don’t get sick from it again. The thinking is that the antibodies formed may have a similar appearance to something in your own body’s cells (such as the myelin on nerve cells or other nervous system tissue). So your immune system then erroneously attacks your own cells as well. What follows is a wide constellation of symptoms, depending on which cells and area of the body are affected. Besides this persistent immune activation and reaction, other theories of possible long-Covid syndrome causes include persistent viral replication, metabolic dysfunction, residual cellular injury from the initial viral infection, and unmasking of underlying diseases which were just under the surface and pushed over the edge by the Covid-19 infection.
What is the treatment for long Covid syndrome?
Treatment for Long-Covid Syndrome is the same as other chronic post-viral syndromes, as well as MECFS symptoms. Unfortunately, this treatment is typically symptomatic, meaning treating the specific individualized symptoms such as insomnia, headache, pain, etc., rather than one unifying treatment. It is important to not automatically consider these patients as “functional”, or that they are embellishing their symptoms. Many of them were highly functioning professionals suddenly stopped in their tracks with this disruptive constellation of symptoms and no one can explain exactly why to them. Thus, anxiety and depression secondary to these symptoms and associated frustration should also be considered. Some patients have reported that their long-Covid symptoms improved after receiving the Covid-19 vaccination, but this has certainly not been a consistency for everyone. Treatment involves a trial and error process of trying different medications, depending on what symptoms are being targeted. For neurological symptoms and headaches, think of it as trying to find something to help “reset” or “reboot” the system electrically. Optimizing nutrition is also important.
How long do long Covid symptoms last?
This is an evolving science and surely more information will come over time. This study of 3762 patients found that the most frequent symptoms after 6 months were fatigue, post-exertional malaise, and cognitive dysfunction. For the majority of patients (>91%), the time to recovery was more than 35 weeks. By 7 months, many patients had not yet recovered (mostly from systemic and neurological/cognitive symptoms), had not returned to previous levels of work, and continued to experience significant symptom burden.
How do you treat Covid-19 headache?
Coronavirus (Covid-19) headache is discussed in much greater detail here in terms of background, symptoms, and treatments. If this is an issue for you, I would suggest that you read that article for a better overall understanding. However, to summarize, there are a few different varieties of Covid-19 headache. Patients that have a history of migraine commonly have a flare up of their migraines related to the Covid-19 infection itself. Similarly, it has been common to see migraines flare up with the Covid-19 vaccine as well. These migraine flare ups are typically temporary and may last a few days to a week or so for some. There is also a milder nonspecific tension type headache (achy pressure tightness) that some patients get with either the Covid-19 infection, or the Coronavirus vaccine, and it is also typically a temporary headache which may last a few days at most. Then, there are the unfortunate group of patients that develop New Daily Persistent Headache (NDPH) after Covid-19 infection, and much more rarely after the Covid-19 vaccine itself. This is a much more persistent headache which begins as a daily persistent headache from the onset, and lasts for more than 3 months. It is notoriously a very resistant form of headache to many treatments. However, improvement is still possible with the combination of time and trial and error treatments until the most effective treatment is found, which can be widely variable between patients.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.