Understanding Acephalgic Migraine
Imagine feeling a migraine attack without any of the migraine pain, just everything else that comes with the migraine. That’s what acephalgic migraine is. These mysterious headaches can cause light and sound sensitivity, nausea, visual disturbances, brain fog and a wide variety of neurological symptoms—without the throbbing head pain that typically comes with a migraine attack. While they may sound like a dream come true for those who suffer from painful migraines, acephalgic migraines can still be disruptive to daily activities.
Acephalgic migraine, also known as silent migraine headaches, migraine aura without headache, or typical aura without headache is considered a “migraine variant”. Silent migraine symptoms are often mistaken for a seizure or stroke and many healthcare providers are not familiar with these disorders. Abdominal migraine and cyclical vomiting syndrome are also forms of silent migraines since they often lack associated headache.
While the pain associated with a regular migraine can be debilitating, acephalgic migraines often go undiagnosed or untreated because the lack of pain may make them seem less severe. However, it is essential to seek medical attention if you are experiencing an acephalgic migraine, as these visual disturbances can still disrupt daily life.
Acephalgic Migraine Causes
So what causes silent migraines? The normal sequence of events in an attack of migraine with aura is that the “migraine switch” turns on in the brain. This can be turned on by a variety of triggers including hormones, stress, foods, weather, or just spontaneously. In those 30% of migraineurs that get aura, there is cortical spreading depression (CSD) — a slow wave of neuronal and glial depolarization across the cerebral cortex. As this electrical wave spreads across the outside of the brain (cortex) at about 2-3 mm per minute, it causes the aura symptoms. Depending on where this wave spreads dictates the type of aura symptoms experienced. The process of aura is described in much greater detail here if you want a much deeper understanding of aura symptoms. Aura symptoms should last 5-60 minutes and are typically followed by the headache phase of a migraine. However, in acephalgic migraine, the pain phase does not develop for unclear reasons.
Silent Migraine Symptoms: Migraine Aura Types To Look For
There are 6 types of recognized migraine aura. The symptoms of silent migraine attacks can vary from person to person but basically include one or more of the following migraine aura symptoms lasting 5-60 minutes, which are not followed by a headache (or sometimes a very mild non-migraine headache).
1. Visual Aura: Visual Disturbances
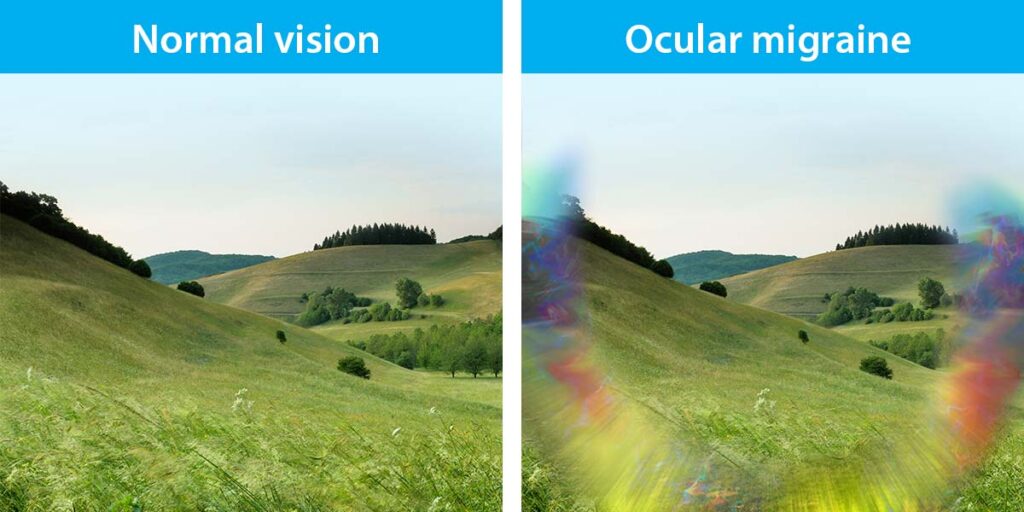
Visual aura is the most common type of migraine aura. These symptoms consist of typical visual aura symptoms such as blind spots, zigzag patterns, flashing lights, fortification spectra, scintillating scotoma, prizms, scotoma (blind spot), geometric shapes, vision loss, and other visual aura that occur with no headache at all. As the cortical spreading depression spreads across the visual cortex in the back of the brain, these visual symptoms are triggered as the neurons are activated from this electrical wave across the brain.
Acephalgic migraines can significantly impact your vision and can be incredibly disorienting. This can cause difficulty driving, concentrating, or performing daily tasks until the symptoms dissipate. While physical pain does not occur, they should still be taken seriously as they can significantly affect day-to-day life.
2. Sensory Aura: Sensory Changes
Sensory aura is the 2nd most common type of migraine aura. These sensory disturbances may include numbness and tingling sensations along one side of the body, most commonly in the face and arm. Some get a perioral numbness and tingling sensation around the mouth. Similar to the mechanism of the visual aura, if the electrical wave of aura spreads across the sensory cortex, these symptoms become evident.
3. Speech and/or Language Aura: Speech and Language Difficulties
Speech or language aura (dysphasia) is the 3rd most common type of migraine aura. These speech and language problems can range from stuttering or difficulty forming words, word finding, slurred speech, or understanding language or speech. Similar to the mechanism of the visual aura described above, if this electrical wave spreads across the speech cortex, these symptoms manifest.
4. Motor Aura: One-Sided Weakness
Motor aura (previously called hemiplegic migraine) is an infrequent form of migraine aura. This may include weakness on one side of the body, difficulty coordinating movements, walking or maintaining balance. Similar to the mechanism of the visual aura described above, if this electrical wave spreads across the motor cortex, these symptoms become evident.
5. Brainstem Aura: Variable Neurological Brainstem Symptoms
Brainstem aura (previously called basilar migraine or basilar artery migraine) is another rare type of migraine aura. To meet criteria for brainstem aura, there must be be at least 2 of the following 7 symptoms present; dysarthria (slurred speech), vertigo, tinnitus (ringing in ears), hypacusis (decreased sense of hearing), diplopia (double vision), ataxia (unsteady walking), and decreased level of consciousness. The mechanism of brainstem aura is not entirely clear, but these symptoms are felt to be caused by transient, reversible dysfunction of the brainstem nuclei which influence these symptoms.
6. Retinal Migraine Aura:
Retinal migraine aura is a rare type of migraine aura with temporary vision loss and is sometimes called optical migraine. It differs from typical visual aura in a few ways. First, symptoms occur in one eye only. In contrast, normal visual aura can occur towards one side of the visual field, but occurs in both eyes to that side. If you close each eye individually, this can help differentiate whether it’s typical visual aura or retinal migraine aura. The mechanism for retinal aura is also not precisely known. There are theories of cortical spreading depression across the retinal layer (which is a layer of nerve cells), but there’s not been clear evidence for this. Limited existing evidence suggests transient vasospasm (narrowing) of the central retinal artery or its branches, causing brief ischemia (lack of blood flow) in the retina or optic nerve head.
Other Possible Symptoms of Acephalgic Migraines
Along with the above symptoms, other possible signs of an acephalgic migraine include symptoms which can occur with any type of migraine. These may include nausea, light and sound sensitivity (photophobia, phonophobia), sensitivity to smell (osmophobia), neck pain, dizziness, fatigue, brain fog, difficulty concentrating, and irritability.
Testing for Acephalgic Migraine
It is important to exclude stroke, TIA, or other pathological secondary causes during initial presentations of acephalgic migraine. Symptoms can appear the same as stroke or TIA and should be treated as such emergently when they first occur. Once a recurrent pattern of similar aura symptoms is established, then the events can be presumably more likely aura. However, if aura symptoms are either new or lasting longer than 60 minutes, they should always be evaluated in the emergency department.
A brain scan should be performed preferably with MRI at some point if symptoms continue to occu, but a CTA brain and carotids is more appropriate in the emergency room setting. Inflammatory labs of ESR and CRP should be checked, especially for visual aura above age 50. A hypercoagulable panel should also be considered. An EEG should be considered to exclude seizure activity.
Acephalgic Migraine Triggers
Acephalgic migraine triggers are the same as for any type of typical migraines.
Stress and Anxiety
Stress and anxiety are some of the most common triggers for any type of migraine, including acephalgic migraines. Mindfulness Meditation, Yoga, Relaxation Techniques, and Cognitive Behavioral Therapy (CBT) can all be beneficial in managing stress and anxiety levels.
Hormonal Changes
Hormonal changes such as those experienced during the menstrual cycle can also trigger acephalgic migraines. Understanding your body’s hormonal cycles and taking steps to manage them can help to reduce your symptoms. This may include tracking ovulation cycles, limiting caffeine intake, avoiding certain foods, exercising regularly, and getting adequate sleep.
Certain Foods and Beverages
Your diet can also play a role in your acephalgic migraine symptoms, and there are many dietary triggers to be aware of. It is essential to ensure that you eat a balanced diet with plenty of fruits, vegetables, lean proteins, and healthy fats. Eating regular meals throughout the day can also help to manage your migraines.
Environmental Triggers
Environmental factors such as changes in weather, bright lights, smoke, or strong smells can also trigger acephalgic migraines. Workplace environmental factors are also important to minimize. Being aware of your surroundings and limiting exposure to triggering environments may help reduce the frequency and intensity of your episodes. Creating eye-friendly workspaces, and the use of migraine glasses to block blue ray light from office lighting and computer screens can be very helpful.
Other Triggers
There are many other possible triggers for acephalgic migraines which can include insufficient sleep, changes in your daily routine, caffeine, among many others. It is important to be aware of all the potential triggers so that you can take steps to manage them and reduce your episodes.
Silent Migraine Treatment: Options And Strategies
Here are some treatment options and strategies if you suffer from acephalgic migraines. An accurate diagnosis is key to optimizing treatment strategies.
Medications
Medication is often the first line of defense for those suffering from acephalgic migraines. Various medications are available to help manage symptoms. However, since there is no pain with acephalgic migraine, the standard abortive options such as triptans, gepants, nonsteroidal anti-inflammatory drugs (NSAIDs), and anti-nausea medications are of little use. If there is a mild non-migraine headache with the aura symptoms, these medicines can be considered. However, there is no effective abortive medicine for migraine aura itself.
Migraine prevention treatments to try to lessen the attacks from happening is the most important strategy for acephalgic migraine.
Lifestyle Changes
Acephalgic migraines can be difficult to manage, but there are lifestyle changes that may help reduce the frequency and intensity of your episodes. Regular exercise, sleep hygiene practices, dietary modifications, and limiting environmental trigger exposure can all play a role in managing your symptoms. Avoiding common migraine triggers is also important. A migraine diary can help with tracking migraine days and possible food triggers or other associations.
Alternative and Complementary Therapies
Traditional medications may not be enough for those suffering from acephalgic migraines to manage their symptoms. Fortunately, there are a variety of alternative therapies that can help treat the condition and provide relief from the pain and other associated symptoms.
Acupuncture, chiropractic care, massage therapy and biofeedback are some treatments available for individuals struggling with acephalgic migraines. Magnesium and Vitamin B2 (Riboflavin) are two of many migraine supplements that can often be helpful in helping to prevent aura symptoms, as well as migraine attacks. Yoga, meditation, hypnosis, and mindfulness can also benefit individuals with acephalgic migraines. These techniques can help reduce stress levels, which can trigger the condition.
Conclusion
In conclusion, acephalgic migraines can be very disruptive to normal function until the symptoms subside, but treatments and strategies are available to help manage the symptoms. Medications, lifestyle changes, alternative therapies, and complementary treatments may all play a role in reducing the frequency and intensity of your episodes. Additionally, avoiding common triggers and practicing self-care techniques can help to reduce the likelihood of triggering an episode. Ultimately, it is vital to work with your doctor to develop an individualized plan of care that best suits your needs and preferences.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.