High altitude headache, also known as altitude headache, commonly affects people who ascend to higher elevations, typically more than 8,000 feet (2,400 meters) above sea level. The reduced air pressure (barometric pressure) and lower oxygen levels at higher altitudes can lead to altitude sickness, of which headaches are a primary symptom.
In this blog post, we will ascend into the symptoms and warning signs of altitude sickness, its three stages, the relationship between high altitude and headaches, how to deal with and treat altitude headaches with conservative measures as well as medicines such as Acetazolamide (Diamox), and learn what to expect for the duration of altitude headaches. It’s essential to understand altitude headaches from altitude sickness to ensure a safe and comfortable experience when traveling to higher elevations.
Onwards and upwards we go…
What are Symptoms or Warning Signs of Altitude Sickness?
As you ascend to the breathtaking realm of higher altitudes, your body may encounter difficulties adjusting to the thinner air and lower oxygen levels. Think of the onset of altitude sickness as a critical signal from your body, urging you to slow down to give your body time to acclimate, because it’s no longer in the low elevation environment that it lives at. This condition manifests through a spectrum of mild symptoms that shouldn’t be ignored because they can lead to severe symptoms requiring medical care.
Initially, you might notice a headache that’s persistent and different from the usual tension type headaches or migraines you may normally get. Accompanying this, feelings of loss of appetite and nausea can emerge, making it hard to keep food down. Dizziness is another telltale sign, and fatigue can be unshakeable even after a full night’s sleep. Diarrhea can also occur. Shortness of breath might catch you off guard, with even mild exertion leaving you gasping for air.
These symptoms serve as crucial indicators, reflecting your body’s distress at the higher elevation because it doesn’t have enough oxygen, nor enough time to acclimate. It’s the body’s way of signaling that it needs more time to adapt to the environment’s reduced oxygen supply. Ignoring these early warnings could lead to more severe complications, emphasizing the importance of listening to and respecting your body’s limits as you navigate the heights.
What are the 3 Stages of Altitude Sickness?
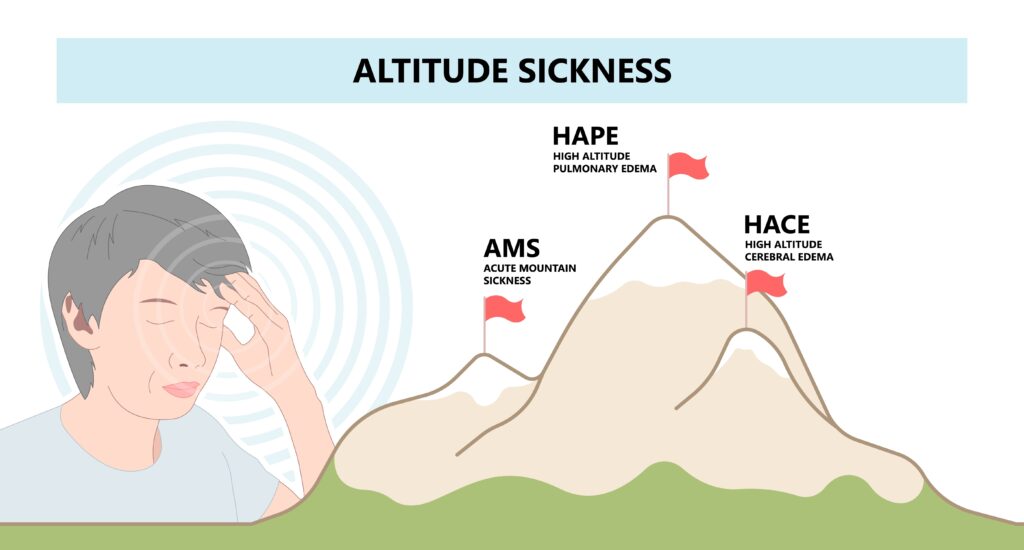
Navigating higher elevations above sea level introduces the body to a spectrum of challenges, culminating in the potential onset of altitude sickness. This condition unfolds in a tiered progression, marked initially by symptoms of Acute Mountain Sickness (AMS), advancing to High Altitude Pulmonary Edema (HAPE), and in its most severe form, culminating in High Altitude Cerebral Edema (HACE). Each stage escalates in seriousness and necessitates a deeper understanding for anyone journeying to high elevations. Avoiding this step-wise progression into severe altitude sickness which can evolve to a medical emergency in severe cases.
AMS serves as the body’s initial alert, manifesting through symptoms like headache, nausea, dizziness, and an overwhelming sense of fatigue. These signs are the body’s plea for time to adjust to the less oxygenated environment. It’s the most common stage and often the first indication that the body is struggling with the altitude change.
Progressing from AMS, HAPE represents a more serious reaction to altitude, characterized by fluid accumulation in the lungs. Symptoms extend to chest discomfort, difficulty breathing, even at rest, making it a condition that demands immediate medical intervention to prevent further complications.
The most severe stage, HACE, involves the swelling of the brain caused by increased pressure. It’s a life-threatening condition marked by confusion, imbalance difficulty walking, and altered consciousness. Prompt medical treatment is critical to manage and reverse the effects of HACE.
Understanding these stages of altitude sickness reinforces the importance of acclimatization and respecting the body’s limits when ascending to higher altitudes. Recognizing the symptoms early on can be lifesaving, underscoring the need for preparedness and caution in high-elevation adventures.
Can High Altitude Cause Headaches?
The phenomenon of experiencing a mild to severe headache at elevated altitudes is indeed a real and often unsettling consequence of the body’s struggle with the lower oxygen levels and decreased air pressure at high elevations. The lower elevation that you live in, the more likely you may encounter high-altitude headache. The intricate balance of oxygen and carbon dioxide in our bloodstream is central for optimal bodily function. When this equilibrium is disrupted, as is common in higher elevation environments, the body undergoes a period of adjustment. Headaches are one of the most common symptoms of altitude sickness, reflecting this period of adjustment.
These headaches serve as a clear indicator from our body, a distress signal of sorts, urging us to either slow our ascent or allow more time for acclimatization. It’s crucial to recognize that these headaches are not just ordinary discomforts, but are indicative of the physiological adjustments our bodies are making in response to the less oxygen-rich air. Paying heed to these signals and responding with appropriate measures can significantly mitigate the discomfort and potential health risks associated with high altitude exposure.
How Do You Deal With Altitude Headaches?
Addressing altitude headaches effectively requires a multifaceted approach that prioritizes your body’s need to adjust to the higher elevation. Ensuring adequate hydration with plenty of fluids is paramount, as dehydration can exacerbate headache symptoms.
The best way to avoid dehydration is to incorporate water and electrolyte-rich drinks into your regimen to maintain fluid balance. A good rule of thumb to avoid dehydration headache is to drink half of your body weight in ounces of water each day. For example, someone weighing 200 pounds should drink 100 ounces of water daily.
Additionally, pace your ascent to higher altitudes; a gradual climb allows your body the necessary time to acclimate, reducing the likelihood of developing headaches. It’s advisable to incorporate a rest day or two into your itinerary, especially after significant elevation gains.
Limiting or avoiding substances that could dehydrate you or disturb your sleep, such as alcohol and caffeine, is also beneficial. Sleep plays a critical role in acclimatization, and disrupting it could worsen headache symptoms.
For immediate relief, consider over-the-counter pain relievers like ibuprofen or acetaminophen, but use only as directed and consult a healthcare provider for guidance, particularly in the context of high altitudes where their effects may vary. You could also consider some home remedies for nausea that can help with that unpopular symptom of altitude sickness. Supplemental oxygen could be considered at a local medical facility if symptoms are severe enough.
Lastly, listen to your body’s signals; if headaches persist despite these measures, allow yourself additional time to acclimate or descend to a lower altitude as needed. This proactive approach to managing altitude headaches can significantly enhance your high-altitude experience, allowing you to enjoy the beauty of those elevated environments, including that outdoor mountainside fire pit at the ski resort more comfortably.
What is the Best Medicine for Altitude Headaches?
Identifying the optimal medication for alleviating altitude headaches requires a personalized approach, taking into account both the severity of symptoms and the individual’s overall health. For many, over-the-counter analgesics like ibuprofen or acetaminophen provide sufficient relief, helping to mitigate the discomfort associated with altitude-induced headaches. These medications can be effective for managing pain, but it’s important to use them judiciously and in accordance with a healthcare provider’s guidance.
In certain scenarios, where prevention of altitude sickness and its symptoms is a priority, prescription medications such as Acetazolamide (Diamox) may be recommended. Acetazolamide works by helping to speed up the process of acclimatization, thereby reducing the likelihood of experiencing headaches due to altitude adjustments. Interestingly, it is also the first line treatment of Idiopathic Intracranial Hypertension (IIH), which is a type of headache caused from high cerebrospinal fluid pressure.
It’s critical, however, to engage with a healthcare professional to determine the most appropriate medication strategy for your specific situation. This conversation ensures that you receive advice tailored to your medical history and altitude exposure plan, optimizing both safety and effectiveness in managing altitude headaches.
How Long Do Altitude Headaches Last?
The duration of headaches resulting from high altitude exposure can differ widely among individuals, influenced by several factors including the rate of ascent, personal health, and the altitude achieved.
Generally, these headaches align with the body’s acclimatization process to the new elevation. For many, relief is found within 24 to 48 hours as the body adjusts to the decreased oxygen levels and lower air pressure. So for that ski trip planning, it’s a good idea to add a couple extra days just to be safe to acclimate and not spend a big part of your trip feeling lousy. If you acclimate quickly without much downtime, then you get some bonus days!
However, it’s important to monitor the progression of symptoms closely. If headaches persist beyond the initial acclimatization period or become increasingly severe, this may signal the need for a more cautious approach, including descending to a lower altitude or seeking medical consultation.
Persistent or intensifying symptoms should not be overlooked, as they could indicate the onset of more serious forms of altitude sickness. Proactive measures, such as maintaining hydration, pacing ascent, and allowing for adequate rest, can play a crucial role in minimizing the duration and impact of altitude headaches.
Remember, each individual’s experience with altitude can vary, and what works for one person may not suit another. Therefore, paying close attention to your body’s response to higher elevations and taking appropriate action based on those signals is essential for a safe and enjoyable high-altitude adventure.
When to Seek Professional Medical Attention
Navigating the challenges of higher elevations, while mostly manageable through acclimatization and proper care, sometimes presents scenarios that demand the expertise of a healthcare professional.
If you find that symptoms such as severe or unrelenting headaches, profound confusion, noticeable difficulty in breathing, or the onset of chest pain emerge, it’s imperative to transition from self-care to professional medical assistance. These symptoms, especially if they escalate or do not improve with initial self-management strategies, may be indicative of more severe forms of altitude sickness, such as HAPE or HACE, which require immediate attention.
It’s essential to recognize the threshold where professional guidance becomes necessary. Acting on the side of caution can prevent altitude sickness from advancing to life-threatening stages. Engaging with a healthcare provider not only facilitates a proper diagnosis but also ensures that you receive tailored advice and treatment that align with your specific medical conditions and altitude exposure.
In the realm of high-altitude adventures, where the body is subjected to significant stress, prioritizing your well-being by seeking medical advice when symptoms escalate is a crucial step in safeguarding your health. Remember, while the journey to high elevations can be exhilarating, ensuring a safe return is paramount!
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.