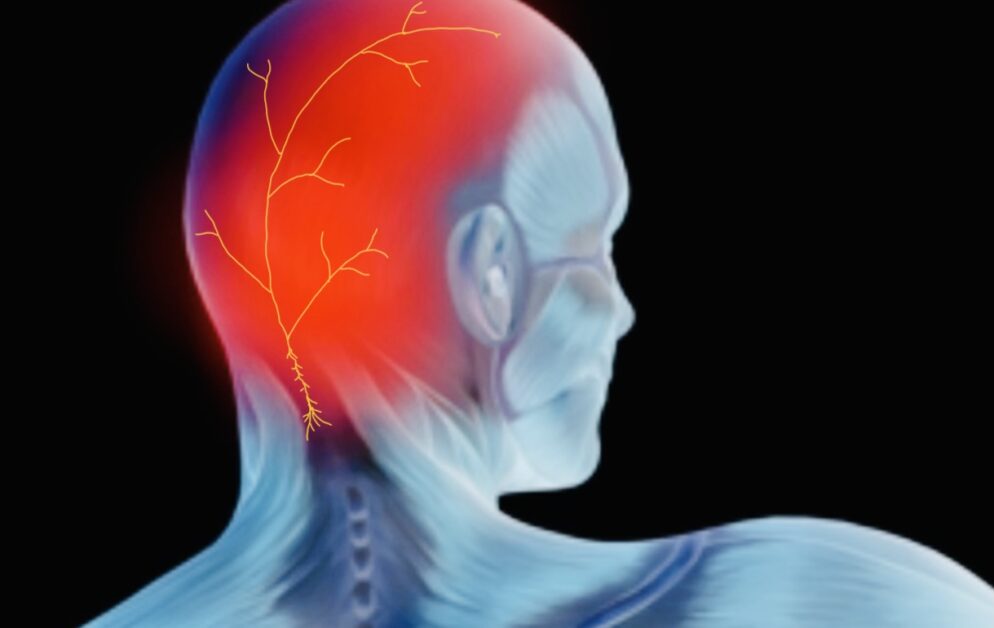
Occipital neuralgia is a headache that causes severe pain in the head’s back, top, and sides. It can be caused by inflammation or damage to the occipital nerves at the base of your skull. The pain can range from mild to debilitating, lasting from a few seconds to several minutes. It can also be a contributing trigger to worsening migraine headaches. Knowing what triggers occipital neuralgia can help you prevent and manage its symptoms better.
TRIGGERS OF OCCIPITAL NEURALGIA
Read on to explore common triggers for occipital neuralgia and strategies for preventing them.
Common triggers of Occipital Neuralgia
The common triggers for occipital neuralgia include physical pressure or trauma to the neck, head, or scalp. This can include sleeping in an awkward position, keeping your head in one position for too long, a traumatic injury to the neck and shoulders, whiplash, neck surgery, surgery to the back of the skull, tight collars or hats that put pressure on the back of your head, and poor posture. There may also be some associated cervicogenic headache.
Other triggers can include stress and anxiety, tension headaches, inflammation around the neck or head, and certain medications. Certain medical conditions such as cluster headaches, migraine, aneurysms, viral infections and sinus infections can also be triggers.
How these triggers can affect the body and cause occipital neuralgia
The triggers discussed above can cause tension and inflammation around the occipital nerve, leading to pain in the back of your head. This pain is often described as sharp or throbbing. It may be accompanied by nausea, sensitivity to light or sound, aching in your neck or shoulders, dizziness, and numbness or tingling in the affected area.
MANAGING TRIGGERS
Strategies for identifying and avoiding personal triggers
One of the best ways to manage and prevent occipital neuralgia is by identifying and avoiding personal triggers. Keeping a symptom diary can help you spot patterns in your symptoms to better identify the things that trigger them. It’s important to note what activities or situations seem to trigger your headaches and any emotions or physical sensations accompanying them.
Other strategies for preventing occipital neuralgia include avoiding tight collars and hats, practicing good posture, sleeping on a supportive mattress, and getting regular exercise. The straps for CPAP machines used at night for sleep apnea can sometimes also put pressure on the occipital nerves and irritate them.
Relaxation techniques such as deep breathing, progressive muscle relaxation, visualization, and yoga can help reduce stress levels to prevent or reduce symptoms of occipital neuralgia.
Having knowledge is key when it comes to staying on top of your health. If you experience any occipital neuralgia symptoms, don’t hesitate to talk with a physician who can suggest tailored remedies that could lessen discomfort and improve well-being.
Tips for managing triggers
Here are some tips for managing triggers and preventing occipital neuralgia:
- Practice good posture and take frequent breaks to avoid strain on your neck and shoulders
- Avoid tight collars and hats that put pressure on the back of your head
- Get regular exercise to reduce stress levels
- Use relaxation techniques such as deep breathing, visualization, and yoga
- Avoid activities or situations that may trigger your headaches
- Stay informed about the condition, and talk to your doctor if you have any concerns.
Stress management techniques
Suffering from occipital neuralgia can be daunting, but stress management offers a way for people to take control of their symptoms. From deep breathing exercises to yoga and visualization, there are multiple methods that individuals can use to manage the pain associated with this condition daily.
Deep breathing is an easy and accessible technique to help manage stress and reduce pain. It involves inhaling deeply through the nose and then exhaling slowly out of the mouth, focusing on a slow and steady breathing pattern.
Progressive muscle relaxation is another technique that helps people relax their muscles by tensing and releasing them one at a time. Visualization techniques involve using your imagination to focus on calming images or positive affirmations. Finally, yoga is a great way to reduce stress and tension while strengthening the body.
Maintaining good posture
Maintaining good posture is important for preventing and managing symptoms of occipital neuralgia. Poor posture often causes tension in the neck and shoulders, which can lead to pain in the back of the head.
To avoid this, sitting up straight with your chin slightly tucked in and your shoulders relaxed is important. You should also avoid slouching and hunching, as these can further strain the neck and shoulders.
When sleeping, it’s important to use a supportive mattress that does not put too much pressure on the head or neck. You should also avoid sleeping in positions that cause your head to tilt back, such as lying on your stomach or using several pillows.
The best position for your head and neck while sleeping is as neutral and midline to the axis of your body as possible (not raised up too high, or too low).
Finally, it’s important to take frequent breaks when sitting for long periods and incorporate stretches into your day to release tension in the neck and shoulders.
Avoiding prolonged inactivity
Prolonged inactivity can lead to increased stress levels, contributing to occipital neuralgia. Staying active and incorporating regular exercise into your daily routine is important to reduce the risk of developing this condition. This can help release tension in the neck and shoulders and reduce stress levels.
PREVENTION IS KEY
Preventing triggers in managing occipital neuralgia
One of the most important steps in managing occipital neuralgia is preventing triggers. By avoiding activities and situations triggering headaches, people can reduce their chances of experiencing pain and other symptoms associated with this condition.
Benefits of lifestyle changes
Making lifestyle changes can be beneficial for managing symptoms of occipital neuralgia. Practicing good posture, avoiding tight clothes and hats, regular exercise, using relaxation techniques, and reducing stress are all important steps in preventing and managing this condition.
It is also essential to stay informed about the condition and talk to your doctor if you have any concerns. Making these lifestyle changes can help reduce pain and improve the overall quality of life.
Regular exercise
Regular exercise is an important part of managing symptoms of occipital neuralgia. Exercise helps reduce stress, tension, and pain while also helping to improve overall physical health. It’s important to find activities you enjoy that don’t put too much strain on the neck and shoulders. Examples include walking, swimming, biking, or yoga.
Proper sleep
Getting enough sleep is essential for preventing and managing occipital neuralgia. It’s important to maintain a regular sleeping schedule, avoid stimulants such as caffeine and nicotine before bedtime, and use a supportive mattress that does not put too much pressure on the neck and shoulders.
Avoiding overuse of electronic devices
Overusing electronic devices can contribute to neck and shoulder pain, so it’s essential to take frequent breaks when using them. It’s also helpful to hold the device at eye level and maintain good posture while using it. Taking these steps can help reduce stress in the neck and shoulders and prevent or manage symptoms of occipital neuralgia.
WHEN TO SEEK HELP
Seek medical attention for occipital neuralgia if you experience any of the following symptoms:
- Headaches that worsen with movement or position change
- Pain in the back of your head or neck that lasts longer than one week
- Numbness, tingling, or weakness in the face, scalp, or neck
- Severe headaches accompanied by vision disturbances, nausea, vomiting, or confusion
If you think you may have occipital neuralgia, you must talk to your doctor as soon as possible. They can diagnose the condition and provide treatments to help manage symptoms. With proper lifestyle changes and treatment, people with this condition can experience a dramatic improvement in their quality of life.
TYPES OF TREATMENTS FOR OCCIPITAL NEURALGIA
Once diagnosed, there are many treatments available for occipital neuralgia. These treatments include medications, physical therapy, occipital nerve blocks, and alternative therapies. Talking to your doctor about the best treatment options for you is important.
Your doctor may prescribe pain relievers or other medications to help manage symptoms of occipital neuralgia. These can include over-the-counter medications such as aspirin and ibuprofen and prescription medications like muscle relaxants or antidepressants.
Physical therapy is an important part of treating occipital neuralgia. It may involve exercises to help stretch and strengthen the neck and shoulders, massage to reduce tension and stress, or hot and cold therapy to help ease the pain.
Your doctor may suggest an occipital nerve block procedure in more severe occipital neuralgia cases. This involves injecting an anesthetic or steroid into the affected area to relieve pain temporarily. Cases that remain refractory to standard treatments may be considered for a surgical procedure called occipital nerve decompression.
Many alternative therapies may help manage symptoms of occipital neuralgia. These include acupuncture, chiropractic care, and biofeedback. Talking to your doctor about the best treatment plan for you is important.
CONCLUSION
Occipital neuralgia is a painful disorder that affects the nerves in the back of the head and neck. It can cause headaches and other symptoms that can be difficult to manage. With proper treatment and lifestyle management, however, people with this condition can experience a dramatic improvement in their quality of life.
If you think you may have occipital neuralgia, you must talk to your doctor as soon as possible to discuss treatment options. With the right care and lifestyle modifications, you can find relief from your symptoms and enjoy life again.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.