
Can a Pinched Nerve Trigger Migraines and Headaches?
Intro Do you suffer from migraines or headaches that just won’t go away? You may be wondering if a pinched nerve is the cause. While

Intro Do you suffer from migraines or headaches that just won’t go away? You may be wondering if a pinched nerve is the cause. While

The mental and physical exhaustion resulting from constant intense pain can be overwhelming. The aching sensations and tension in your neck and shoulders can damper
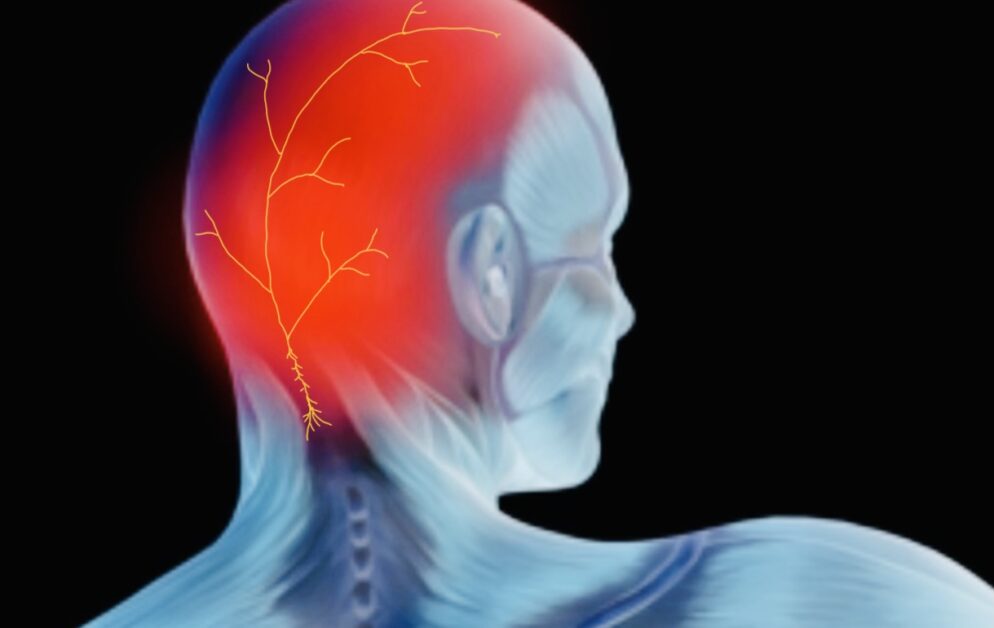
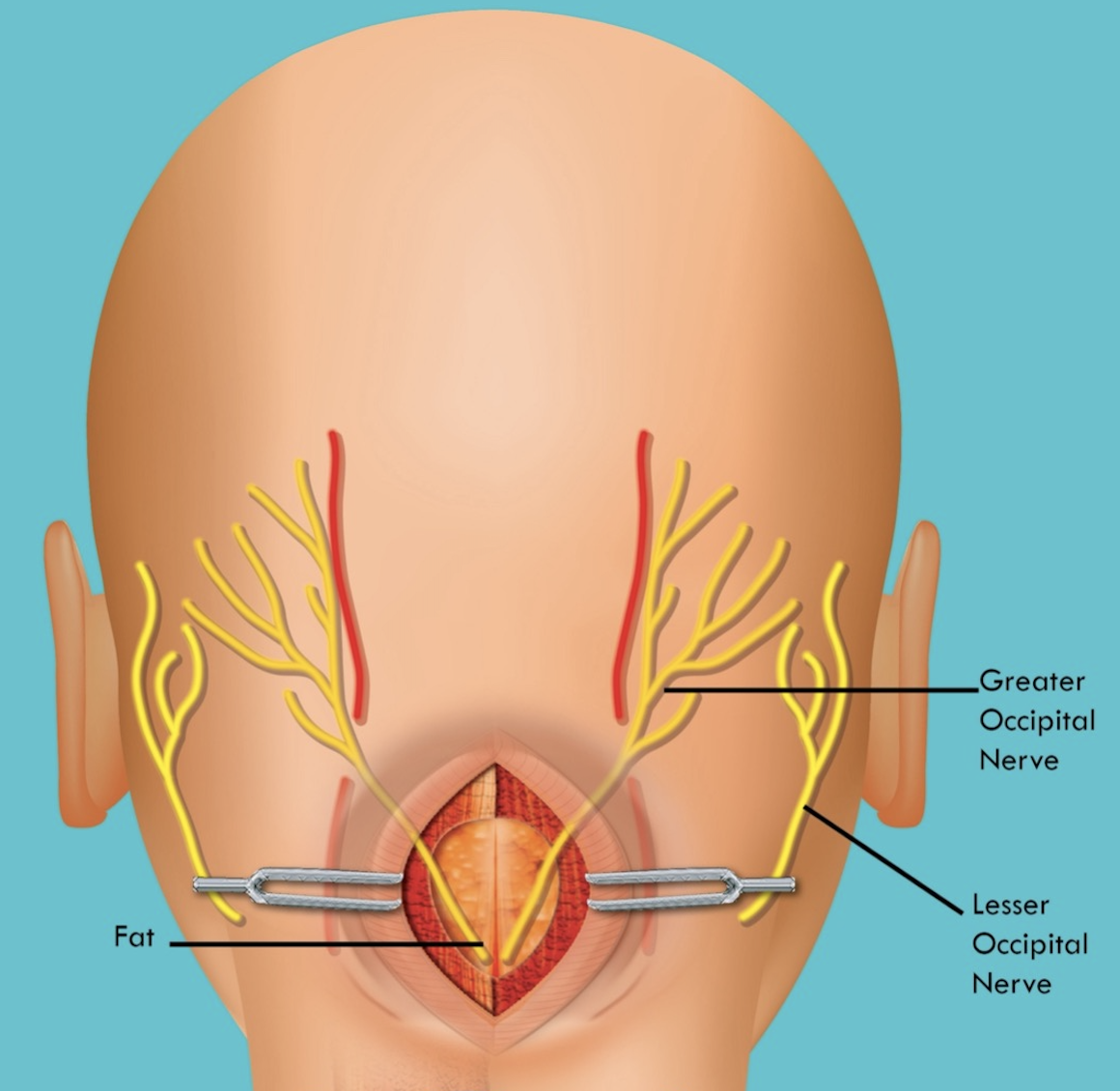
Occipital neuralgia is a headache that causes severe pain in the head’s back, top, and sides. It can be caused by inflammation or damage to
Occipital neuralgia can be a miserable pain in the back of the head, discussed in much greater detail here. If you’re reading this blog article,

Do you frequently wake up with a headache? This is a common feature with several types of headache disorders, but they are all distinct headache
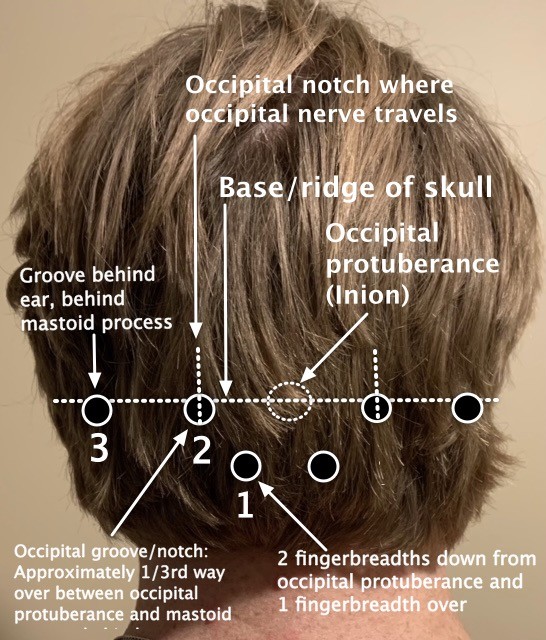
Occipital Neuralgia Symptoms, Causes, and Treatments Occipital Neuralgia Symptoms What is occipital neuralgia? Occipital neuralgia can be a severe pain and headache in the
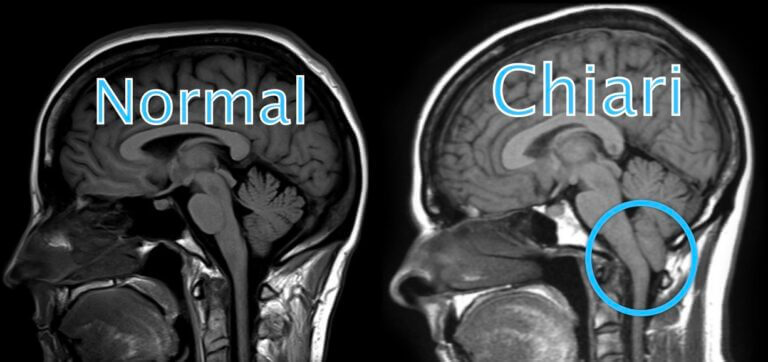
What Is Chiari Malformation? Chiari malformation, also known as Arnold-Chiari malformation, is a common congenital (born with it) condition of anatomical variation involving the brain