TMJ Disorder and Headache: Understanding the Connection
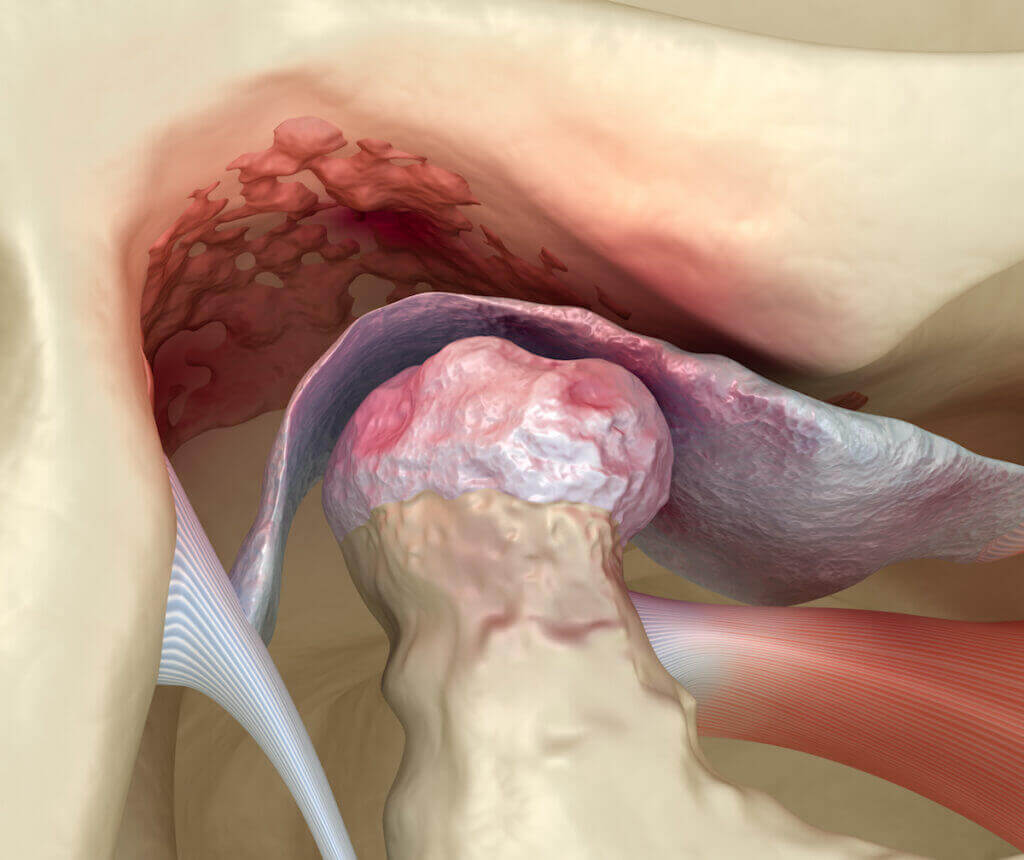
The temporomandibular joint (TMJ) is the joint that connects the jawbone and the skull. This is one of the most powerful joints in the human
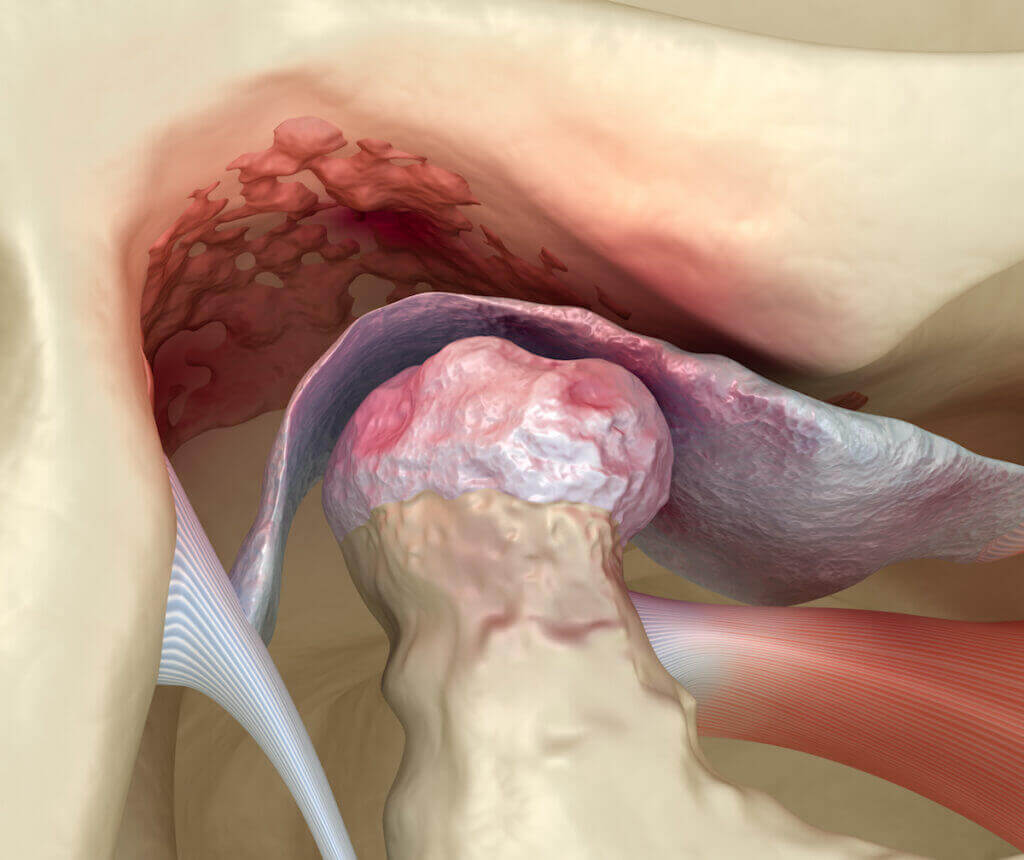
The temporomandibular joint (TMJ) is the joint that connects the jawbone and the skull. This is one of the most powerful joints in the human

While the exact cause of migraines remains unknown, the neurovascular theory of migraine is currently most accurate. Regardless of exact mechanism, there are many different

Migraines are a very intense type of headache that are often accompanied by other symptoms, including nausea, vomiting, sensitivity to light and sound, as well

According to the World Health Organization, headaches are a global problem, affecting people of all races, income levels, and regional areas. Headache disorders impact about

I see patients in our headache center from all over the United States and from many other countries. Many patients travel hundreds of miles by

Migraine is a very disruptive disorder to have to deal with. It interferes with your family, work, financial, social, and educational lives. When the burden

What are the neuromodulation devices available for migraine headache treatment, and what are the differences? There are 5 main migraine neuromodulation devices available. They are

Pure menstrual migraine and menstrually-related migraine are very common forms of migraine, often referred to generically as hormonal headache. Overall, migraine is estimated to effect

Chronic daily headache being endlessly fueled and driven by rebound headache (medication overuse headache or MOH) is one of the most common headache disorders that

Imitrex vs. Maxalt, Zomig vs. Maxalt, Amerge vs. Relpax, Frova vs. Imitrex, Maxalt vs. Relpax, Zomig vs. Imitrex, Frova vs. Amerge, Imitrex vs. Treximet. Maxalt