Understanding migraine triggers is crucial for anyone who suffers from migraines. Identifying what triggers your migraines can often feel like a daunting task, as triggers vary significantly among individuals. Some people may find that stress, menstrual cycles, or certain foods bring on an attack, while others might be sensitive to environmental factors like weather changes, bright lights, or loud noises. This blog post aims to educate you on the various common and uncommon migraine triggers and offer practical strategies for identifying and managing these triggers effectively. By doing so, you can reduce the frequency and severity of your migraine attacks and improve your quality of life. Long term exposure to migraine triggers can evolve your occasional episodic migraine into daily chronic migraine, so you certainly want to avoid this with the correct strategies.
Understanding the Common Triggers of Migraines
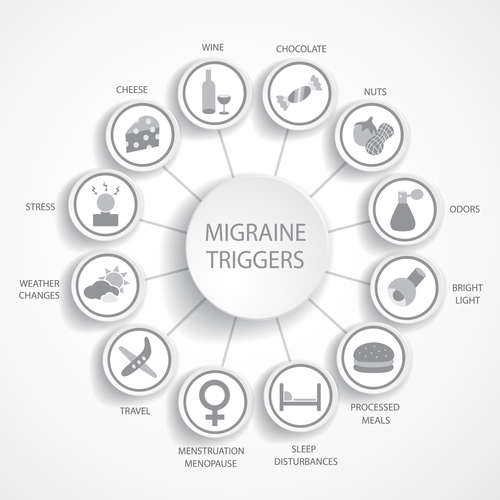
Migraines can be multifaceted, with triggers varying widely among individuals. Common migraine triggers include hormonal changes, stress, bright lights, loud noises, food additives, and environmental factors such as weather changes or air pollution. Some triggers can be more elusive such as the smell of chicken cooking 5 houses down, or strawberry ice cream, as a couple of my patients had discovered.
For some, these triggers might operate in combination, making it even more challenging to determine what is causing their migraines. Their migraines may be activated by a combination of triggers, enough to “push them over the edge”, rather than a single trigger. For example, the start of a menstrual cycle may be enough of a migraine trigger for one woman. Yet for another woman, her menstrual cycle may lower her migraine threshold, but not enough to fully trigger the attack. However, if she then adds a stressful event and a barometric pressure change from a bad thunderstorm, that combination of triggers may then be enough to lower her migraine threshold even more and the migraine attack then breaks through.
Factors like lack of sleep and barometric pressure changes can play a significant trigger role for many. To effectively manage migraines, it’s important to grasp this complexity and recognize how these elements may be interacting. Using a migraine triggers list can be an invaluable tool in tracking and identifying the unique factors that affect you.
However, as I always explain to my patients, there doesn’t “have” to be a trigger. Migraine can just happen. Migraine is an electrical disorder. Similar to epilepsy, another but different type of electrical disorder, seizures can also just happen without a trigger. For some, their migraines can similarly happen unexpectedly without an identified trigger.
Hormonal Changes and Migraine Triggers in Women
Hormonal fluctuations are a prominent trigger for many women experiencing migraines. This hormonal influence is why 1 in 5 women (20%) have migraines, as opposed to 1 in 16 men! Variations in estrogen levels, particularly around menstrual cycles, pregnancy, perimenopause, and menopause, can significantly contribute to the pattern of migraine attacks.
These hormonal changes can lead to migraines, making it essential to monitor your menstrual cycle and note any associated symptoms. This vigilance can offer valuable insights into how hormonal shifts may be influencing your migraines. For some women, preventive medications or specific lifestyle adjustments can help mitigate these hormonal triggers. They are many strategies that can be used in treating menstrual migraine. Discussing these options with a healthcare professional can provide personalized strategies to manage this aspect of your migraines effectively.
Migraine Food Triggers and Dietary Causes of Your Migraines
Dietary choices can significantly influence migraine occurrences, with certain foods and eating habits known to be common culprits. Some of the most notorious migraine food triggers include aged cheeses, processed meats, chocolate, red wine, and foods containing additives like MSG, nitrites and nitrates.
In addition to specific foods, irregular eating patterns such as skipping meals or fasting can also provoke migraines. Maintaining a food diary can be an effective tool to pinpoint dietary triggers. By documenting what you eat and noting the timing of migraine attacks, you can identify patterns and correlations. A dietary trigger will most often trigger the migraine the same day it is consumed, and often shortly after. However, it could potentially still correlate the following day.
If certain foods consistently appear to be linked with your migraines, it may be beneficial to eliminate them from your diets (migraine elimination diets). Consulting with a nutritionist can provide personalized advice to help you make informed dietary choices that minimize your migraine risk. Remember, every individual’s triggers are unique, so a tailored approach is key to effective management.
The Role of Stress and Lifestyle in Triggering Migraine Attacks
Stress is a well-documented catalyst for migraine headaches, acting as both a trigger and an amplifier of symptoms. Emotional stress from work, relationships, or significant life changes can precipitate an attack, while physical stress from overexertion or illness can do the same. Identifying stressors in your life is a critical first step in mitigating their impact on your migraines.
Incorporating effective stress management techniques is crucial. Mindfulness practices such as meditation and deep-breathing exercises can help regulate your emotional state and stress levels, reducing the likelihood of a migraine. Regular physical activity, like yoga or walking, not only alleviates stress but also promotes overall well-being.
Sleep hygiene is another vital aspect to consider. Lack of sleep and sleep disorders such as obstructive sleep apnea and insomnia are common migraine triggers, so maintaining a consistent sleep schedule can make a significant difference. Avoiding screens, caffeine, and alcohol before bedtime and creating a restful environment can improve sleep quality and lessen the misery of migraine pain.
Daily routines should also include balanced nutrition and hydration. Skipping meals or dehydration can exacerbate stress and trigger migraines. Setting aside time for regular, nutritious meals and drinking plenty of water throughout the day can be beneficial.
Finally, consider seeking professional advice for stress management strategies tailored to your specific needs. A healthcare provider or therapist can offer personalized guidance, helping you to develop a comprehensive approach to managing stress and, by extension, your migraines.
Environmental Factors and Their Impact on Migraines
Environmental factors can play a significant role in triggering migraines for many individuals. Weather changes, particularly shifts in barometric pressure, are frequently cited as culprits. These changes can cause physiological responses that may set off a migraine. I always say that patients with migraine can predict the weather more accurately than they do on TV weather forecasts! Air travel is another common migraine trigger given the barometric pressure changes involved during an airplane ride.
Similarly, exposure to bright lights, whether from the sun or artificial sources like screens and fluorescent lighting, can also provoke an attack. Flashing lights, seeing light reflected off a car, or shining between fences while driving in a car can be enough of a trigger for some people. Utilizing protective measures such as wearing sunglasses outdoors, the use of migraine glasses or reducing screen brightness can help mitigate these triggers. Visual related environmental migraine triggers are often prevalent in the work environment, but there are measures to consider in creating eye-friendly workspaces.
Loud noises are another common environmental factor that can contribute to migraines. Whether it’s the constant hum of city life or sudden loud sounds, auditory stimuli can exacerbate symptoms. Some people love concerts, but for others with migraine it can be a torture chamber. Investing in noise-canceling headphones or finding quieter spaces can be effective strategies to manage this trigger.
Strong smells and strong odors, often overlooked, can also impact migraine sufferers. Strong perfumes, cleaning products, or even certain foods can act as triggers. Identifying and avoiding these scents can make a noticeable difference in managing your migraines and associated migraine symptoms such as nausea, sensitivity to light and sound. That one guy at work that seems to bathe in his cologne is often the least favorite person of the migraine patient working in the same office.
Indoor air quality is another factor worth considering. Poor ventilation or exposure to pollutants like smoke and chemical fumes can trigger migraines in some people. Using air purifiers and ensuring good ventilation can help improve the quality of your indoor environment, reducing the likelihood of a migraine attack.
How To Figure Out Your Migraine Triggers. Keeping a Migraine Diary to Track and Identify Triggers
Keeping a migraine diary is a highly effective strategy for identifying your unique migraine triggers. This simple yet powerful tool involves recording various aspects of your daily life to detect patterns and correlations with migraine occurrences. Start by documenting the date and time of each migraine attack, along with details about your activities, food and drink intake, sleep quality, emotional state, and any environmental factors you were exposed to such as weather changes, bright lights, or Aunt Sally’s nagging questions at the family birthday party on why you aren’t married yet.
Additionally, note any medications or supplements you take and their effects on your symptoms. Over time, this detailed log will help you pinpoint specific triggers, whether they are dietary, hormonal, stress-related, or environmental. Regularly reviewing your migraine diary with a healthcare provider can offer further insights and assist in tailoring a personalized management plan. Consistency is key, so make it a habit to update your diary daily, even on migraine-free days, to get the most accurate and comprehensive understanding of your triggers.
How Do You Control a Migraine Trigger? Effective Strategies for Managing Identified Migraine Triggers
Controlling migraine triggers requires a multifaceted approach tailored to the unique factors identified through careful observation and tracking. Dietary modifications are often necessary when specific food or food additives are pinpointed as triggers, such as monosodium glutamate (MSG). This might mean avoiding aged cheeses, processed meats, or other items known to provoke your migraines. Aiming for a healthy diet with whole foods and limiting processed refined foods, sugars, and chemicals can be game-changing. For stress-induced migraines, incorporating stress management techniques such as mindfulness meditation, regular exercise, and adequate sleep can be highly effective.
Environmental triggers, such as bright lights or loud noises, can often be managed by making simple adjustments to your surroundings. Using migraine sunglasses to reduce glare, employing noise-canceling headphones, or improving indoor air quality with purifiers are practical steps you can take. Hormonal fluctuations, particularly in women, may require a combination of lifestyle changes and medical interventions; discussing options like preventive medications with your healthcare provider is crucial.
For those triggered by weather changes or barometric pressure shifts, staying informed about weather forecasts and minimizing exposure during significant fluctuations can help. There are apps that some migraine patients use to alert them of significant barometric pressure shifts and they can treat preemptively. For those triggered by the barometric pressure changes associated with an airplane ride, taking a “mini prophylaxis” abortive medicine prior to take off can be very helpful. Additionally, a headache diary can continue to be an invaluable tool for refining your understanding of these triggers and assessing the effectiveness of your strategies. By consistently implementing these tailored interventions, you can significantly reduce the frequency and severity of your migraine attacks.
The Importance of Professional Medical Advice for Migraine Management
Navigating the complexities of migraine triggers can be overwhelming, underscoring the importance of good medical advice from healthcare professionals, particularly a headache specialist. While self-tracking and lifestyle adjustments are invaluable, they are no substitute for the comprehensive assessment and personalized treatment plan that a healthcare provider can offer. Medical professionals can employ diagnostic tools to rule out other potential causes of your headaches and provide guidance tailored to your unique situation.
For instance, preventive medications may be recommended based on your specific symptoms and triggers. These medications can be crucial in reducing the frequency and severity of migraine attacks, particularly when lifestyle changes alone are insufficient. In addition, having an effective abortive (acute) medicine to take and knock out the attack when it begins is crucial. In cases involving vertigo migraine triggers or complicated hormonal interactions, professional intervention becomes even more essential.
Additionally, a healthcare provider can guide you in managing co-existing conditions, such as anxiety or depression, which often accompany chronic migraines and can exacerbate symptoms. They can also help you interpret data from your headache diary, offering insights you might overlook and adjusting your treatment plan accordingly.
Remember, managing migraines is not a one-size-fits-all approach; it requires ongoing adjustments and professional oversight. By collaborating with a medical expert, you can ensure that your strategies are both safe and effective, ultimately leading to a better quality of life. Always prioritize medical guidance as a cornerstone of your migraine management plan.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.