I see the worst of the worst headache, migraine, chronic migraine, facial pain, fibromyalgia, and chronic pain from many states and countries. I see patients who have been debilitated by pain, patients whose pain has destroyed their family, marriage, work life, social life, and the ability to function normally. They are void of hope and have lost all self-esteem and confidence, replaced by depression and seclusion. They hide in the shadows of life. They come into the office with dark sunglasses, hoods up, appear detached, soft-spoken with little to say, and have fully committed themselves to the mindset that they will never get better. And they won’t because they don’t allow their brain to develop the plasticity to escape out of that mindset and behavior. We’ll talk about this concept and brain plasticity more later. I have seen patients who slide into this mindset commit suicide because they see no way out. These patients are rampant and come from all walks of life; professionals such as attorneys to blue collar workers to the jobless.
It is an equal opportunity nightmare of chronic pain syndromes. These patients evolve from a once normal life and function to one of minimal to no ability to function normally in life, career, or relationships. I have seen plenty of people pull out of this described rut of a chronic pain lifestyle. It’s possible, but it takes work. Most importantly, it takes the step of convincing yourself that it is possible and will be done, and then readjusting your behaviors, mindset, and thought process accordingly. Give yourself no other option than improvement and realize that there is always hope for improvement. The placebo response in clinical trials involving pain patients (and similar in other subgroups) averages around 30%! That means on average, 30% of pain patients will develop significant improvement despite taking a placebo (fake) treatment. This happens because they convince themselves that they are using the new treatment, and thus they convince their mind that they are improving, and they do! Your mind is the most powerful weapon in your battle against your chronic pain, so learn to use it to your advantage.
Let me be clear that chronic pain is real, it is valid, it can be debilitating, it shouldn’t be ignored or overlooked, it can validly negatively impact all aspects of life which can be out of the control of the patient. I profoundly empathize with these patients. However, there is a lot that is in control of the patient which they often do not realize, and that is my purpose for this blog article. Specifically, they do not realize that they are creating a self-fulfilling prophecy of never improving in pain or function, directly related to their behavior and mindset. No, this discussion doesn’t apply to everyone and all cases, but I would say it does apply to the majority of patients.
Many of these patients create websites, blogs, and social media accounts dedicated and centered around their chronic pain experiences. Their chronic pain becomes their persona, and who they are. It redefines them. This can certainly be helpful to others to learn about similar pain experiences and to feel that they are not alone, and I think it is fantastic that other patients can have these outlets and sources to share their experiences. However, it can also become a dominating way of life which dissolves away any thought, hope or attempt at improving their pain and overall function. These patients get to a point where living any other way besides centered around their chronic pain would seem abnormal to them. They focus their life, their daily activities, their restrictions, their abilities, and their relationships around their chronic pain. It defines them and dictates their life. They are chained and restrained from this focus. This behavior begins to feed into itself and they continue down a path where there becomes no chance at improvement because they don’t allow their mindset or focus to see that as a valid option, and thus do not initiate behavioral changes to try to influence positive changes.
This phenomenon is also reflected in patients who have chronic daily headache, chronic pain, chronic neck pain and whiplash syndrome related to a motor vehicle accident, work related injury, or some other event where they were injured. If there is litigation (lawsuit) involved, it is well known as a clinical predictor that they will rarely improve, because of potential secondary gain (financial, disability, etc.) from their pain, which their subconscious maintains focus on. There have been studies supporting this correlation as well. This phenomenon is not seen in other countries which are not as litigious and ready to sue over anything. We used to have a large unique chronic pain rehabilitation program which was very effective and helpful to many patients. A large focus of this program was on behavioral changes to influence improvements in overall pain and functional abilities. However, patients were excluded from entry if they were involved in any ongoing lawsuit related to their pain, because these patients invariably never got better until the lawsuit was settled and done, and it would be much more beneficial and cost effective to them after legal issues were resolved. We would then admit them following the conclusion of their legal battles if they continued to have chronic pain issues. I have seen many patients reverse their course from that dark reclusive patient scenario described above with the right mindset and approach.
How does pain behavior influence brain plasticity and your chances of improvement?
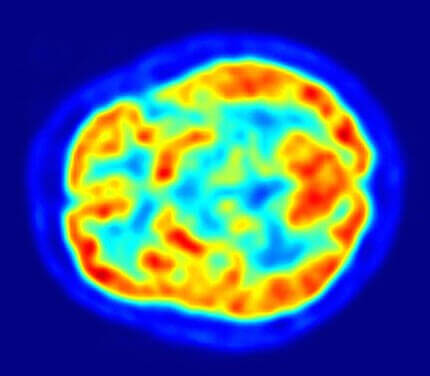
Anatomically and physiologically, this reclusive and socially isolated behavior and mindset of telling yourself that it is impossible for pain to improve or that one cannot function and live a normal life with chronic pain becomes a self-fulfilling prophecy. DON’T LET THAT HAPPEN!! This is solidly based in scientific and biological evidence. Behavior influences cellular, molecular, and physiological changes in the body and brain. Studies have shown that behavior (such as pain limiting behavior, social avoidance, etc.) causes structural and circuitry changes in the brain, which can be lifelong. Social behavior can also cause changes in the brain, although this can be more reversible. These structural changes in the brain and the circuitry of the brain, influenced by behavioral changes (behavioral neuroscience) and mindset, are called brain plasticity. Essentially, plasticity refers to the nervous system’s ability to constantly modify its organization, structure, function, and circuitry connections in response to experiences, behavior, and an endless list of other influencing factors such as pain, stress, diet, emotion, medications, and many other things. Brain circuits related to chronic pain overlap with circuits involving anxiety, depression and some mood disorders. Mood disorders such as depression can affect the plasticity of chronic pain, and likewise chronic pain can influence plasticity of depression and other mood disorder circuitry.
Treatment and conclusions of chronic pain
Treatment is difficult, requires patience, and involves treatment trial and errors (if one treatment doesn’t work, another is tried). The single most important treatment involves you, your behavior in how you respond to your pain, your mindset, and attitude which all in turn influence your brain plasticity positively, and chances of improvement. Do not let your pain define who you are and what you are able to do. Expectations are important in that you should realize that (typically) there is no quick fix or “cure” (but if you stumble across one, which can happen, great!). Learning to live, deal, and function with the chronic pain is vital. If you realize this and make it a primary goal, it can in turn lead to improvements over time by modulating your brain plasticity and electrical circuitry. Most preventive treatments can take 2-3 months to see effects, and there is no way to expedite that. Hang in there and be patient.
Chronic migraine, fibromyalgia, and some other chronic pain syndromes often cluster together. The way to look at these types of chronic pain syndromes is that the neurological system is “hyperactive”, “overactive” or “hypersensitive”. So, the goal is to try to “turn down the volume” of this “hypersensitive” neurological system with medications or other types of treatments. Never conclude that there is no possibility of improving. Remain active physically, socially, emotionally, and maintain active relationships. Treating depression or mood disorders is very important, and a good psychiatrist can make a big difference with this. Chronic migraine and chronic daily headache should have appropriate treatments which may include preventive treatments, CGRP mAb once monthly treatments, supplements and natural therapies, neuromodulation devices, eliminating rebound (medication overuse headache), and using appropriate abortive (as needed) therapy such as triptans, gepants and ditans. Most importantly, remain hopeful. There is always hope and there are constantly new types of treatments becoming available. You can do this!!!
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.