What Is Chiari Malformation?
Chiari malformation, also known as Arnold-Chiari malformation, is a common congenital (born with it) condition of anatomical variation involving the brain tissue inside the back of the skull (cerebellum). It is characterized by the lower part of the brain at the base of your skull descending down into the foramen magnum (normal opening of the spinal column where the spine meets the skull). It is most often a benign and asymptomatic congenital condition found incidentally during routine imaging of the brain when an MRI or CT is done for other reasons (usually headache). However, there are also more rare cases which can lead to compression of the brain stem and the upper part of the spinal cord. This can disrupt the normal flow of cerebrospinal fluid and cause severe symptoms such as muscle weakness, double vision, severe headaches, balance problems, difficulty swallowing, problems with the cranial nerves, and other neurological symptoms.
When the MRI scan findings do not show significant compression at the back of the brain (perhaps just a mild Chiari), and the physical exam does not reveal neurological deficits, it becomes a bit more cloudy. This is the most common scenario. The difficulty is often trying to associate the patient’s symptoms with the Chiari malformation vs. another type of headache disorder such as migraine, chronic migraine, and occipital neuralgia which can all have overlapping characteristics with Chiari. Internet searching will give you a very long list of reported symptoms caused by Chiari malformation (you can probably find about any association you are looking for), although most of the time these associations are inaccurate. This blog addresses the most common and benign of the types of Chiari malformations; type 1.
How Is Chiari Malformation Diagnosed?
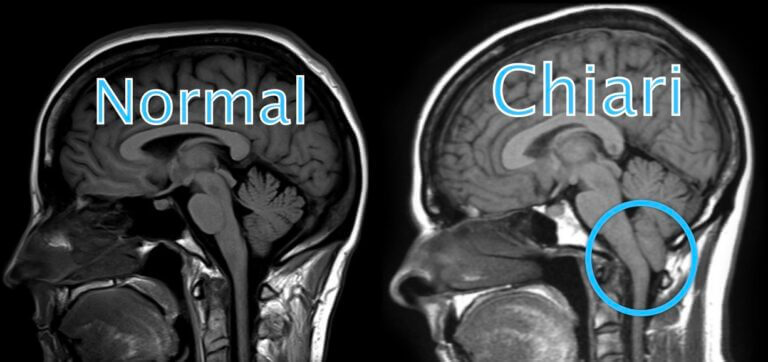
Chiari malformation that is truly related to a patient’s symptoms typically include a “pegged” appearance of the cerebellar tonsils (back and bottom part of the cerebellum) which are pointed rather than rounded, suggesting compression at the cervicomedullary junction (area where the brainstem and upper cervical spinal cord merge between the bottom of the skull and upper cervical spine). It often has a “crammed” appearance when the bottom of the cerebellum appears “crammed” into the upper cervical spine.
The illustration below highlights this appearance compared to a normal brain. When this appearance is present, the patient often does have symptoms that correlate to the Chiari. Unfortunately, most of the time the Chiari malformation is not as extensive, making it more difficult to determine if some of the patient’s symptoms are correlated or not.
A contrast brain MRI which includes a cine flow (cine-phase contrast) study can be helpful in determining the extent of compression and subsequent blockage of normal cerebrospinal fluid (CSF) flow throughout the craniocervical junction. A cervical MRI without contrast is also recommended to rule out a cervical syrinx (enlarged area in the center of the spinal cord), which can sometimes be associated with Chiari. If a cervical syrinx (widening in the center of the spinal cord) is found, an MRI of the remaining thoracic and lumbar spine should also be performed. A CT scan is inadequate for evaluation of Chiari.

In general, Chiari malformation cerebellar tonsillar descent is considered to be within normal anatomical variation in the following:
First decade (0-10 years): 6mm or less
–Second and third decades (10-30 years): 5mm or less
–Fourth-eighth decades (30 to 80 years): 4mm or less
–Ninth decade (greater than 80 years): 3mm or less
Some mild or borderline Chiari malformations can be associated with extensive symptoms, while other times an extensive Chiari malformation is found, but the patient lacks any Chiari symptoms. So, a detailed history of symptoms including headache and associated features is crucial in determining whether a Chiari malformation is clinically relevant or not. This is more useful than basing treatment decisions purely on the extent of tonsillar herniation in Chiari. History is also important in excluding other disorders which can cause a reversible “pseudo-Chiari”, caused by a different disorder such as intracranial hypotension CSF leak, or low-pressure headache) or idiopathic intracranial hypertension (IIH) (previously known as pseudotumor cerebri).
What Are Chiari Malformation Symptoms?
According to the International Headache Society, Chiari headache caused by Chiari type I malformation is usually occipital or suboccipital (back of head/base of skull), of short duration (less than 5 minutes) and provoked by cough or other Valsalva-like maneuvers (straining in the abdominal region such as when having a bowel movement). Notably, Chiari headaches, or cough headaches, are the most classic of the symptoms of Chiari malformation, along with neck pain. Of course, there are other headache disorders that can also cause these characteristics too though. Ultimately, accurate diagnosis is based on the overall symptoms, history, physical exam, and MRI findings. According to the International Headache Society, the Chiari headache should remit after the successful posterior fossa decompression treatment of the Chiari malformation.
Here are the diagnostic criteria and a Chiari malformation symptoms checklist:
International Headache Society diagnostic criteria require Chiari malformation to have at least two of the following:
1. Either or both of the following:
a) Headache has developed in temporal relation to the Chiari or led to its discovery
b) Headache has resolved within 3 months after successful treatment of the Chiari
2. Headache has one or more of the following three characteristics:
a) Precipitated by cough or other Valsalva-like maneuver
b) Occipital or suboccipital location
c) Lasting less than 5 minutes
3. Headache is associated with other symptoms and/or clinical signs of brainstem, cerebellar, lower cranial nerve and/or cervical spinal cord dysfunction. (These may include symptoms such as hoarseness, slurred speech, swallowing or choking difficulty, unsteadiness, dizziness, vertigo, tongue weakness, trigeminal or glossopharyngeal neuralgia, tinnitus, absent gag reflex, facial numbness, autonomic symptoms (syncope, slow heart rate (bradycardia), drop attacks), loss of pain and temperature sensation of the upper torso and arms (from syrinx), loss of muscle strength in the hands and arms (from syrinx).
According to International Headache Society criteria, the diagnosis of Chiari malformation by MRI requires a 5-mm caudal descent of the cerebellar tonsils or 3-mm caudal descent of the cerebellar tonsils plus crowding of the subarachnoid space at the craniocervical junction as evidenced by compression of the CSF spaces posterior and lateral to the cerebellum, or reduced height of the supraocciput, or increased slope of the tentorium, or kinking of the medulla oblongata.
Treatments For Chiari Headache
There are certainly patients with Arnold Chiari malformations that fit the criteria above and truly have a symptomatic Chiari malformation. Those patients with a fairly straight forward history, symptoms, and MRI without other overlapping headache disorders can often do quite well with a successful surgical treatment. The standard surgical treatment is called Chiari decompression surgery, where the lower base of the skull is removed.
Be sure to exclude and treat other associated headache disorders to get a clear view of what symptoms are truly from Chiari vs. other treatable headache disorders!!!
Unfortunately, we see many patients who have had Chiari decompression, but they continue to have chronic daily headache which often resembles their pre-surgery headaches. When you delve deeper into their pre-existing headaches, many times they describe headaches which had/have migrainous features (throbbing, pounding, pulsating pain quality with nausea (+/- vomiting) and/or photophobia and phonophobia (sensitivity to bright light and loud sound with bad headache flares)). These pre-surgical headaches often fit criteria for chronic migraine, many times of which were likely sustained as chronic daily headache and chronic migraine due to medication overuse headache (rebound).
So, if any of the history is suggestive of a migrainous component as above, this should empirically treated for first to ensure they won’t get a cranial surgery/decompression simply for chronic migraine! With that said, if it is an obvious prominent Chiari with clear Chiari headache type symptoms, this can certainly expedite the treatment plan.
Most of the time, the chronic daily headaches that patients continue to have after decompression surgery are associated with some variable degree of these migrainous characteristics. They typically resemble a chronic migraine pattern, and many times treating the headaches as chronic migraine rather than being distracted and treating only as ongoing Chiari headache can provide significant improvement.
If the Chiari has been decompressed, then it is certainly no longer a “Chiari headache” at that point, and treatment and diagnoses should be reconsidered. However, as mentioned above, even more important is screening for these migrainous features prior to surgery, and if present, treatments targeting migraine and chronic migraine should always be exhausted first because pure Chiari headache is not going to cause migrainous features of throbbing, pounding, pulsating headache with nausea (+/- vomiting) and/or photophobia and phonophobia.
Pure Chiari headache just doesn’t cause those symptoms. Those symptoms are migraine. It is common that patients can have both Chiari and migraine. The key is differentiating which is which and eliminating the migrainous component to get more clarity of how much of the symptoms are truly Chiari related, if any.
In addition to a chronic migraine appearing headache, patients who have had Chiari decompression frequently have associated occipital neuralgia in the back of the head and a component of chronic post-craniotomy headache. However, this can also be present prior to surgery and can be another mimic of Chiari headache. This is related to scarring of the tissues in the back of the head and base of the skull where the occipital nerves travel. This scarring can pull, twist, and tangle up the occipital nerves over time which causes persistent occipital pain in the back of the head.
Post-craniotomy headache is technically similar to chronic post-traumatic headache since decompression surgery is, well, certainly a form of trauma to the head. Chronic post-traumatic headache itself commonly has a chronic migraine clinical appearance (with or without pre-existing migraine history), and treating as such can often be very beneficial. For example, we often seen concussion patients that develop chronic daily headache and chronic migraine which is “turned on” by the injury or head trauma.
Successful treatment with significant improvement of chronic daily headache with chronic migraine characteristics following Chiari decompression surgery is often a difficult task requiring patience and a good headache specialist.
Daily medications used in migraine prevention should be considered, particularly ones that are good for not only migraine, but also occipital neuralgia and musculoskeletal pain such as anticonvulsants (topiramate, gabapentin, etc.), TCAs (amitriptyline, nortriptyline), or SNRIs (duloxetine, venlafaxine ER).
Neck physical therapy can often be very helpful at stretching out the suboccipital tissues and lessening tension on the occipital nerves. If there are any migraine or chronic migraine features, then more aggressive migraine preventives such as Botox (OnabotulinumtoxinA) injections , gepants, or the CGRP monoclonal antibodies should also be considered. Botox should be done according to the “PREEMPT protocol”. I prefer to do additional dosing over the occipital nerves (which are virtually always irritated after Chiari decompression) and often add numbing medicine such as bupivicaine which can provide additional temporary relief as the Botox starts to kick in over the next couple weeks.
If there is an ongoing chronic daily headache driver from rebound headache (medication overuse headache), it is also crucial to eliminate this factor. Improvement will not happen while this is an ongoing factor (especially if there is a chronic migraine component). If there are migrainous features to headache exacerbations, then using more migraine specific abortive (as-needed) meds such as triptans, gepants (Nurtec, Ubrelvy, Zavspret) or ditans (Reyvow) should also be considered. Notably, the gepants do not cause medication overuse headache (rebound headache).
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.
FAQ
This is a condition, present from birth, when brain tissue in the back of the brain (cerebellum) extends into the upper cervical (neck) spinal canal. Most cases do not cause symptoms or problems. Treatment usually involves monitoring, surgery if it is causing symptoms, or medication to help manage the pain.
Chiari malformation is not a rare condition. In fact, Chiari information is thought to impact less than 1 out of every 1,000 people. Chari tends to be diagnosed in adults aged 25 to 45.
The true cause of a headache from Chiari malformation is complex, and there are several variables that factor in, such as history of other headache disorders and how much obstruction to cerebrospinal fluid there may be. These headaches tend to occur because of abnormalities in the flow of cerebrospinal fluid. Specifically, if the normal flow of cerebrospinal fluid is obstructed due to the Chiari, it can cause pressure build up and headaches. People who suffer from these headaches tend to have some improvement after surgery or other treatments, but improvement depends on the degree of cerebrospinal fluid flow obstruction and the presence of other headache disorders (such as migraine).
These headaches feel unique and distinct. They tend to originate in the lower base of the skull, but can radiate to the neck and shoulders, and into the head. They can be brief in nature, have a pulsating sensation, and resemble occipital headaches. Classically, there may be a cough headache, or headache that comes on quickly with similar activities such as laughing, straining, or bending over. If the Chiari malformation is extensive, there can be other neurologic symptoms such as numbness and tingling in the face, numbness in the neck into shoulders, dizziness, vertigo, or other problems with cranial nerves.
A procedure called a Chiari decompression will remove bone from the back of the skull to create more room for the brain. This surgery is successful for most people. According to the NIH, 84.2% of people experience success with this surgery. Most people, 86.9%, will experience an improvement in their headaches.
There are other treatments for Chiari malformation that can help alleviate the symptoms as well as the headaches. A cervical laminectomy involves removing a section of your upper vertebrae. Another treatment option is CSF diversion, which involves placing a shunt to channel excess cerebrospinal fluid.
There is also a minimally invasive decompression that will remove excess bone from the skull. The minimally invasive method allows patients to heal faster and this is becoming one of the most common methods for dealing with Chiari malformation.
Some people will experience a return of Chiari symptoms after their surgery. This is for two different reasons:
- The procedure didn’t entirely relieve the pressure at the base of the skull.
- Scarring after the surgery can create conditions where Chiari symptoms actually return.
- There may have been other headache disorders that were mimicking Chiari headaches, or contributing to headaches in the same areas such as undiagnosed or untreated migraine or occipital neuralgia.
The severity and intensity of Chiari malformation headaches will vary from person to person. Most people will experience the same type and severity of their symptoms over their lifetime. However, as we age, our tissues change. Changes in tissue that occur with natural aging can make Chiari malformation, including headaches, sometimes worse over time, but sometimes can also improve.
Overall, there is an excellent outlook for people with Chiari malformation. As mentioned above, over 80% of patients report success with the decompression procedures available, when done in the appropriately selected patient. According to the NIH, only about 17% of patients will need a second Chiari procedure. Headaches also improve in most patients, with very few reporting them after they have healed from their procedure.