
Facial Pain, Headaches, and Migraines: Exploring the Connection
Have you ever experienced sudden pain in your face and head that comes on without any warning? One side of the head might be pulsating

Have you ever experienced sudden pain in your face and head that comes on without any warning? One side of the head might be pulsating

Headaches and sweating are common symptoms that many women experience during pregnancy. These symptoms can be uncomfortable, but there are several ways to manage a

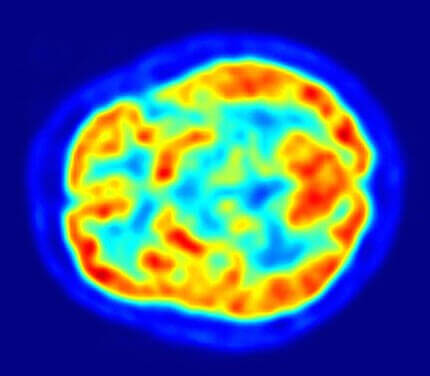
Migraine is a complex neurological condition that can present with various symptoms, including headache, nausea, sensitivity to light and sound, and visual disturbances. Migraine stages

Have you ever felt so overwhelmed by emotions that they caused physical pain? Maybe you experienced a stomachache or headache when feeling anxious or angry.

Headaches can feel like a never-ending throb or other pain somewhere in the head – and this prevents you from focusing and carrying out your

The best migraine diet is… Well first, there are many well established migraine triggers. The beverages and foods that we consume play a role in

The likelihood of a headache increases during the summer months. According to a recent study which surveyed ER visits for headaches, every 9°F rise in

If you experience headaches every day, you likely have a condition known as chronic daily headache. Generally speaking, the difference between episodic and chronic headaches
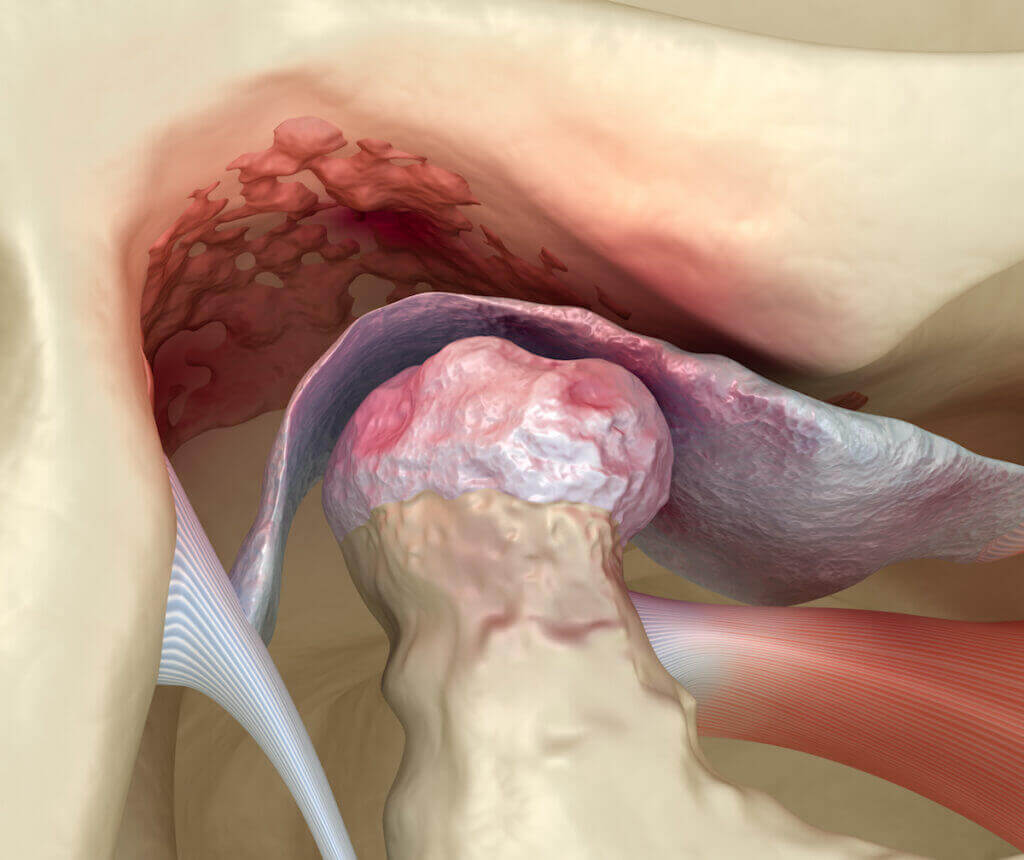
The temporomandibular joint (TMJ) is the joint that connects the jawbone and the skull. This is one of the most powerful joints in the human
I see the worst of the worst headache, migraine, chronic migraine, facial pain, fibromyalgia, and chronic pain from many states and countries. I see patients