What is a Cerebrospinal Fluid (CSF) Leak?
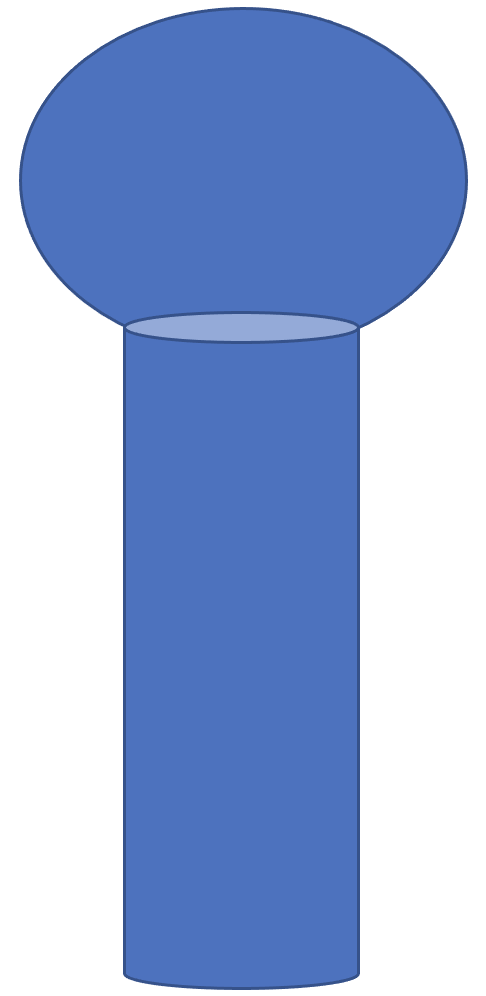
Imagine a thick plastic wrap (like Saran wrap) in the shape of an elongated tube, continuous with a widening at the top into the shape of a basketball. Now, imagine the inside of this entire plastic wrap enclosure filled with water, so it is very firm anywhere you push on it.
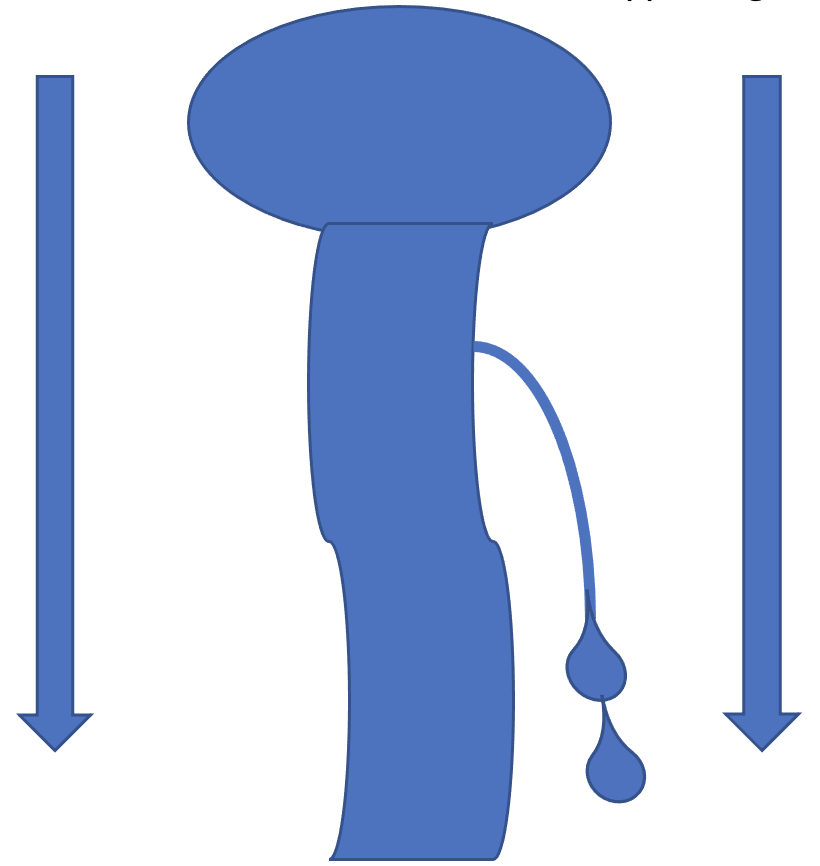
Then, imagine you take a pin and poke a hole in it and water starts to seep out. The pressure on the inside then decreases due to the leak, and the basketball appearing structure at the top begins to sag.
Now you understand the basic pressure dynamic concept of a CSF leak.
Now, imagine this water filled plastic wrap structure is surrounded and protected by the vertebrae of the spinal column and the skull. Inside the spinal canal and skull, this layer of plastic wrap represents a thick membrane called the dura mater. It is a continuous layer lining the inside of the spinal canal and continues along the inside lining, nooks, and crannies of the skull.
Instead of water, this dura mater membrane is filled with cerebrospinal fluid (CSF). This system keeps the CSF pressure within a certain normal range. The purpose of this CSF enclosed system is to cushion and keep the spinal cord and brain afloat.
Similar to the plastic wrap example above, if there is a small leak in this dura mater membrane, CSF escapes. Intracranial pressure and intraspinal pressure within this system then decreases. The result of the CSF leak is intracranial hypotension with subsequent sagging of the brain (instead of the basketball structure), and the spine.
Congratulations. You now understand the concept of a CSF leak. That’s the easy part though. The difficulty is understanding why it developed, how to visualize and test for the specific location of the leak, and most importantly, how to seal the leak. We’ll talk about all of this.
What Causes a Cerebrospinal Fluid (CSF) Leak?
CSF leaks are most often spontaneous CSF leaks, meaning they just happen without clear reason.
Spinal CSF leaks can also be associated with injury or trauma, lumbar puncture, facet osteophytes (bone spurs along the spine), disc herniations, intracranial hypertension (IIH; pseudotumor cerebri), connective tissue diseases (Ehlers-Danlos syndromes, etc.), diverticuli/perineural cysts along the spine, CSF-venous fistulas, hemangiomas, and bariatric surgery.
Some CSF leaks can occur through a leak in the sinuses. These patients may have clear (many times excessive) drainage coming from the nose, and sometimes the ear. Ear nose and throat (ENT) doctors often evaluate for these types of leaks. They have the patient collect fluid from the nose and it is tested for CSF.
As mentioned, the most common form of CSF leak overall is from spontaneous intracranial hypotension (SIH). SIH is when someone randomly develops a CSF leak, often for no reason. SIH is what this blog article will primarily focus on.
What is Considered Low CSF Pressure (Intracranial Hypotension)?
ICHD3 criteria state that intracranial hypotension (low CSF pressure) is considered less than 6 cm CSF (60 mm CSF or H2O) when opening pressure is checked on a lumbar puncture.
Who Gets Cerebrospinal Fluid (CSF) Leaks?
CSF leaks can occur in any age, and in both sexes with a predilection for women (63%).
What Are the Symptoms of a Cerebrospinal Fluid (CSF) Leak?
A large systematic review and meta-analysis of published data revealed the following frequencies of symptoms associated with CSF leaks:
-Headache (97%)
Headache is the most common symptom of a CSF leak and occurs in 97% of patients. However, 3% may NOT have any headache!
Of those that do have a headache, 92% of them are the classic orthostatic headache (positional headache). This means that the headache comes on when you are standing and improves when you are lying down. The other 8% of headaches are non-orthostatic headache (they may not have a positional/orthostatic character).
The headache location for a CSF leak in order of frequency is most often occipital (33%), diffuse throughout the head (30%), frontal (21%), fronto-occipital (11%), or temporal (8%).
-Nausea/vomiting (54%)
-Neck pain and stiffness (43%)
-Other ear-related symptoms (33%)
May include ear fullness, hyperacusis (everything sounds very loud).
-Hearing disturbances (28%)
May include muffled, echoed, or distorted hearing.
-Dizziness (27%)
-Tinnitus (ringing in ears) (20%)
-Vertigo (17%)
-Reduced level of consciousness (15%)
-Other visual symptoms (14%)
May include blurred vision, nystagmus, visual loss.
-Back pain (14%)
Cervical radiculopathies have also been reported, as have numbness and tingling in the face, back of the head, and upper arms.
-Photophobia (sensitivity to light) (11%)
-Movement disorders (10%)
These can manifest as gait disorder, Parkinsonism, ataxia, dysarthria (slurred speech), tremor, bradykinesia (slowness of movements), poor balance, chorea.
-Diplopia (double vision) (6%)
One-sided (unilateral) or both sides (bilateral) 6th cranial nerve palsy is most common if there is a cranial nerve palsy. A 3rd, 4th, or multiple cranial nerve palsies are less common. With that said, all of these findings are quite rare.
-Cognitive symptoms (6%)
May include cognitive impairment, behavioral changes, memory, and/or slow thinking.
Where Are the Most Common Locations of Cerebrospinal Fluid (CSF) Leaks in the Spine?
A large systematic review and meta-analysis of published data revealed the following frequencies of location:
-Thoracic spine (41%)
-Cervicothoracic junction (25%)
-Multiple locations (24%)
-Cervical spine (14%)
-Lumbar spine (12%)
What Do You See on a Brain MRI When There is a Cerebrospinal Fluid (CSF) Leak (Intracranial Hypotension)?
The best test to start with when a CSF leak is suspected is a brain MRI with contrast. This will often show some of the classic features of CSF leaks. The brain MRI findings occur because of the brain sagging down (recall the leak dynamics discussed above). The most common features of a CSF leak on a brain MRI are:
-Diffuse pachymeningeal enhancement (73%)
Imagine the sagging brain pulling down on the dura mater membrane which is attached to the inner skull lining. This causes inflammation and irritation of this layer, and it usually will light up with contrast on the MRI. The result is diffuse, smooth, non-nodular pachymeningeal enhancement.
Keep in mind that sometimes if the MRI is done too early after the CSF leak develops, it may not show this enhancement yet. The reason is because there hasn’t been enough time to allow the inflammatory process to develop.
-Venous engorgement (57%)
As the brain sags downward, the venous channels are also pulled downwards. This enlarges the inside of the veins and thus more blood collects in them. Engorgement of the epidural venous plexus can also be seen, as well as the transverse sinus venous distension sign.
-Brain sagging (43%)
Following a CSF leak, the spinal fluid pressure decreases. Without the CSF cushioning and keeping the brain and spinal cord afloat, gravity has its way and pulls the brain downwards. Thus, you get the sagging brain.
Signs of this on an MRI can be seen in a variety of often subtle ways including flattening of the ventral pons, descent of the cerebellar tonsils (pseudo-Chiari), partial effacement of basal cisterns, inferior displacement/flattening of the optic chiasm, reduced mamillopontine distance, thinning of suprasellar cistern, obliteration of prepontine cistern, and decreased ventricular size.
-Pituitary gland enlargement/hyperemia (38%)
Without the normal CSF pressure pushing the pituitary gland down within its sella (the “cave” where the pituitary sits), the pituitary tissue is able to expand upwards when the CSF pressure is low. This can cause it to appear more plump or full.
-Subdural collections (subdural hygromas) (35%)
These are fluid collections between the dura mater lining inside the skull and the arachnoid later covering the brain. This fluid is made up of a variable mix of CSF, protein, and sometimes blood from tearing of the stretched little veins traveling between these membranes due to the downward traction.
-Normal brain MRI (19%)
Some patients appear to have a perfectly normal brain MRI. Therefore, a normal brain MRI does not exclude the possibility of having intracranial hypotension. Diagnosis really comes down to putting together all the clinical symptoms along with test results. If there is a strong suspicion for a CSF leak based on symptoms, then further imaging may be pursued (as detailed below).
What Are the Best Tests to Find a Cerebrospinal Fluid (CSF) Leak?
As mentioned above, the best test to start with when a CSF leak is suspected is a brain MRI with contrast. The subsequent tests to consider when looking for further evidence of a CSF leak, or to localize the specific area of the leak are outlined below. However, not all of these tests are universally available. The available options and preferences will vary between institutions depending on test availability and personnel to perform these diagnostic tests.
-Brain MRI With and Without Contrast
This is the initial imaging test for a suspected CSF leak. Brain MRI with contrast has been shown to be the most sensitive in detecting signs of intracranial hypotension (CSF leak).
The contrast is really key here to look for that pachymeningeal enhancement described above. Unfortunately, brain MRI does not give any information about the location of the CSF leak in the spine (but can if the leak is coming from the sinuses). So, if there is evidence of intracranial hypotension on the brain MRI, it needs to then be followed up by spine imaging to locate the site of the CSF leak.
-Spine MRI With or Without Contrast, With Heavily Weighted T2 Imaging (CSF Leak Protocol)
A spine MRI is usually the next step in identifying the location of the CSF leak and looking for fluid collection along the spine. There are two obvious benefits of this spinal MRI compared to going straight to CT myelogram. First, you do not need to puncture the dura mater (and risk then actually creating a CSF leak when there may not even be one present). Second, it does not require IV contrast. However, if there are no contraindications to having contrast, it may be worth adding it.
-CT Myelogram
If conservative management and/or blood patch fails (discussed below) despite the MRI showing evidence of a CSF leak, a CT myelogram is a good consideration to pursue next to further localize the CSF leak. If spine MRI does not show a CSF collection outside of the spine, then a CT myelogram is also suggested as a next step to localize and help confirm the CSF leak.
Of note, if the spine MRI does show a CSF collection outside of the spine, then a fast CSF leak is likely present, and a conventional CT myelogram may not be able to identify the exact leak site. In this scenario, it is usually higher yield to move directly to a dynamic CT myelogram, or a digital subtraction myelogram (DSM) because these will be better at finding the exact leak site in a fast CSF leak. These two tests are described in more detail below.
CT myelography is done by doing a lumbar puncture and injecting CT contrast into the CSF under fluoroscopy. Then, the patient is taken to the CT scanner to obtain CT images of the spine to look for the specific location of the CSF leak along the spine.
This has often been an effective test for showing the precise location of the leak. However, it is more useful in slow leaks as opposed to fast leaks from large dural tears or multiple leaks. With fast CSF leaks, the injected contrast material spreads over multiple spinal levels before the CT can be completed, and this makes the exact leak site difficult to visualize. Digital subtraction myelography (DSM) or dynamic CT myelography are more useful for localizing fast leaks.
The downside of CT myelography (or any myelography) is that it requires a lumbar puncture, which then poses the risk of developing a CSF leak. So, if there isn’t actually a current leak, there’s a chance that one could develop from the procedure, although this isn’t common.
-Dynamic CT Myelography (Hyperdynamic CT Myelogram)
If the spine MRI DOES show a CSF collection outside of the spine, there is a high probability of a fast leak. In that case, going straight to a dynamic CT myelogram (or a DSM) rather than a conventional CT myelogram is suggested because it will likely be higher yield in identifying the exact CSF leak site.
A dynamic CT myelogram is basically the same as a CT myelogram, but the timing of the procedure is different. Like a CT myelogram, CT contrast is injected into the CSF. However, the CT imaging is done simultaneously with the contrast injection into the CSF rather than a delay between contrast CSF injection and the CT images being taken.
Dynamic CT myelography is done in the lateral decubitus (laying on your side) and/or the prone (on your stomach) position. Some institutions do both sides of the spine on separate days to avoid excess contrast dye load.
Dynamic CT myelogram is often very useful in finding the exact location of a CSF leak, especially in fast leaks from a herniated disc or tear in the dura mater from an osteophyte.
-Digital Subtraction Myelography (DSM)
If the spine MRI does NOT show a CSF collection outside of the spine, and/or a conventional CT myelogram does NOT identify a leak site (or a CSF-venous fistula could be present but not visualized), a lateral decubitus DSM is often the next best step.
If the spine MRI DOES show a CSF collection outside of the spine, a fast CSF leak is likely present. In that case, either a DSM or dynamic CT myelogram should be considered over a conventional CT myelogram since these will be more likely to visualize the exact leak location. If there is an extradural CSF leak on MRI, then a prone DSM is usually done first. If this is negative, then a lateral decubitus DSM is the next step.
A DSM is basically a CT myelogram under fluoroscopy while digitally subtracting pre-contrast images which then enhances the contrast visibility. It is very helpful in visualizing CSF-venous fistulas which often do not show up on other MR or CT spinal imaging, especially when done in the lateral decubitus (lying on your side) position. Lateral decubitus DSM is helpful in cases of CSF-venous fistula as well as nerve root sleeve tears, or a herniated disk or osteophyte (bone spur) tear in the dura mater layer.
DSM requires breath holding or is done under general anesthesia to stop breathing for a short time to prevent movement artifact. A limited number of published cases have shown a very high sensitivity (100%) for identifying the exact CSF leak site.
It has been suggested that DSM is particularly useful in localizing three types of CSF spinal leaks:
1) Rapid leaks which can be seen on MR or CT myelography as extensive longitudinal extradural CSF collections.
2) CSF leaks in front of (ventral) the spinal cord.
3) CSF-venous fistulas between the spinal epidural veins and the subarachnoid space that are not visualized on MR or CT myelography. In one study, CSF-venous fistulas were found in 1/5th of patients with refractory intracranial hypotension with no identifiable CSF leak on spinal imaging.
-MR Myelogram
This is the same concept as a CT myelogram except that it is done with an MRI and gadolinium (MRI contrast) is injected into the CSF by a lumbar puncture instead of CT contrast. It has excellent contrast resolution and there is no radiation exposure involved. However, intrathecal gadolinium is an off-label use. MR myelography can also be performed without gadolinium injected into the CSF (intrathecal injection), but the diagnostic yield may be better with contrast.
The unconventional use of intrathecal gadolinium (injected into the CSF) is not commonly available. A limited number of published cases have shown a high sensitivity (75.5%) for identifying the exact CSF leak site. MR myelogram can be particularly helpful in looking for slow CSF leaks. However, intrathecal gadolinium has also been reported to cause neurotoxicity at higher doses. Furthermore, more recent studies have suggested that it may not be better overall compared to MR myelography without intrathecal gadolinium and there is some debate about this.
-Radionuclide Cisternography (Radioisotope Cisternogram)
This test is a type of nuclear medicine imaging. It is performed by injection of a radionuclide tracer material by lumbar puncture into the CSF. Then images of the brain and spine are taken at certain intervals up to 24-72 hours to watch for the movement of the nuclear tracer.
A cisternogram assesses for abnormal CSF flow and is quite sensitive for detecting if there is a spinal CSF leak. However, it doesn’t provide information about the specifica location of the leak. Therefore, it is not done as commonly as it had been in the past for a couple reasons. First, it does require a lumbar puncture which introduces the risk of a CSF leak if not already there. Second, if there is evidence of a CSF leak, it doesn’t help in localizing where it is in the spine. Therefore, if a lumbar puncture is being performed, it’s better to get more “bang for your buck” with a test which will be more likely to show the location of the CSF leak so it can then be treated more precisely.
-MR Cisternography
This is not a common test and is sometimes a consideration for evaluating suspected CSF fistulas along the skull base.
-Lumbar Puncture (LP)
It is not common that an LP alone is done to check opening pressure for the sole purpose to determine the presence of a CSF leak. If a lumbar puncture is done and the dura is going to be pierced, it just makes sense to combine it with one of the above diagnostic tests.
If an LP is done to check opening pressure, it should be done in the lateral decubitus position (lying on your side) for an accurate reading. This is especially important when evaluations for elevated CSF pressure from idiopathic intracranial hypertension are being evaluated.
Notably, a study showed that opening pressures in CSF leaks are not always low. In CSF leaks, opening pressure was found to be low (less than 6 cm CSF) in 67%, normal in 32% (6-20 cm CSF), and high normal (greater than 20 cm CSF) in 3% (highest noted was 22.8 cm CSF). Technically, the ICHD3 criteria for high CSF pressure is greater than 25 cm CSF. Regardless, the point is that the opening pressure result alone is not an absolute of whether a CSF leak exists or not.
Of note, some patients may actually have idiopathic intracranial hypertension (IIH, or pseudotumor cerebri) as the primary underlying problem. They may fluctuate between periods of high CSF pressure (IIH) until it springs a CSF leak in a weak point in the dura mater membrane, and then low CSF pressure until the leak seals. They may go back and forth between these phases.
How Do You Fix and Treat a Cerebrospinal Fluid (CSF) Leak?
-Conservative Management
The first line treatment for a CSF leak is conservative treatment. This is effective in 28% of patients, without the need for any other treatments. Conservative treatments include bed rest, hydration, pain medications, caffeine, steroids, and avoiding strenuous activity or exertional maneuvers.
-Epidural Blood Patch
If conservative treatments fail, then an epidural blood patch is the next step. What is a blood patch? This is an easy quick treatment in which some of your own blood is first collected. Many institutions combine fibrin glue to the blood in hopes of a stronger seal. That blood is then injected within the spinal canal (but outside of the dura mater membrane) in the region where the CSF leak is suspected. Sometimes it is injected with fluoroscopic XR guidance, and other times without it. The theory is that as the blood clots, it will seal up the leak.
The first epidural blood patch is successful 64% of the time. Large epidural blood patches (more than 20 mL) had better success rates at 77% compared to small epidural blood patches (less than 20 mL) at 66%.
Targeted (blood patch done at a precise spinal level) and nontargeted (blood patch done at a more regional area of the spine) blood patch techniques have shown similar successful results. Targeted blood patches were successful 70% of the time, while nontargeted blood patches were successful 69% of the time.
-Surgical Repair of Dural Defects, Meningeal Diverticula, or CSF-Venous Fistulas
It is uncommon that these types of treatments are needed. However, if the above treatments are not successful, and the type of CSF leak is appropriate for surgery, these may be considered. Surgery may include suturing or packing the tear, ligating or clipping of nerve roots, or paraspinal vein embolization.
What Are the Complications of a Cerebrospinal Fluid (CSF) Leak Repair?
Complications with a CSF leak repair are uncommon. Potential complications could include accidental dural puncture with blood injected into the CSF, arachnoiditis, nerve root compression, compression of the thecal sac (the “tube” structure described at the beginning which encloses the CSF), infection, or attempting to inject the blood patch into an area where there is no space for the blood patch to go (such as bad arthritis, prior spine surgery, scarring).
What is Rebound Intracranial Hypertension After Treatment of Cerebrospinal Fluid (CSF) Leak?
Rebound intracranial hypertension occurs when the CSF pressure starts to get too high after the CSF leak has been sealed. It has been reported to occur between 7%-27% of patients and begins within 24-48 hours of CSF leak repair.
This headache is usually worse in the morning or when lying down. The location of the pain often migrates from the back of the head to the face, like a mask. This uncommon event is more likely in younger women who are obese or those with a fast CSF leak with extradural CSF noted on the prior spine MRI. Rebound intracranial hypertension does not appear to be associated with blood patch level, blood patch volume, or opening pressure.
Rebound intracranial hypertension is usually mild and most often resolves on its own. When treatment is needed, options include acetazolamide, topiramate, methazolamide, furosemide, hydrochlorothiazide, spironolactone, triamterene, and ethacrynic acid. Rarely it can lead to papilledema requiring more aggressive treatments such as repeat lumbar punctures, lumbar drain for 5 days, stents or VP shunting.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.