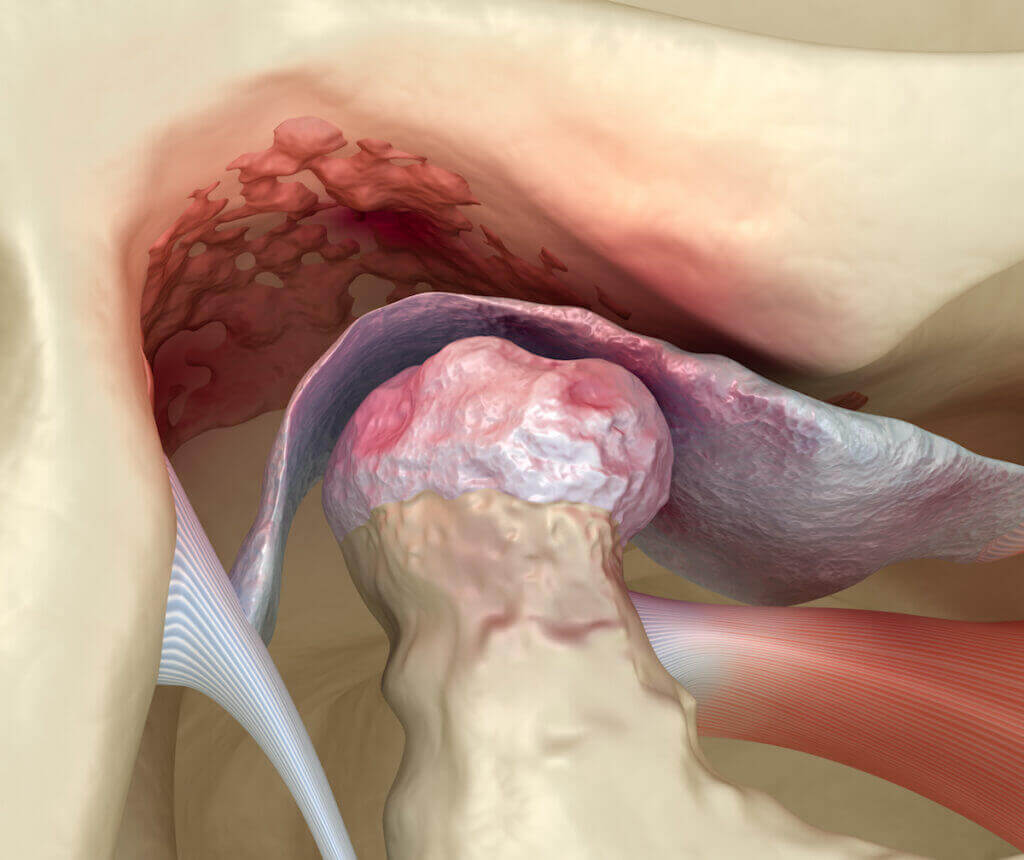
The temporomandibular joint (TMJ) is the joint that connects the jawbone and the skull. This is one of the most powerful joints in the human body, as it can apply 162 pounds per square inch when a person bites.
It is important to realize that the TMJ is a synovial joint. In other words, it is a joint composed of a capsule filled with synovial fluid. Similar to a knee joint (but on a much smaller scale), the synovial fluid keeps the joint lubricated and healthy. However, this can also be the source of various types of dysfunction. There is a condition called TMJ disorder that can contribute to facial pain and headaches. TMJ disorder is fairly common, impacting about 12% of Americans at any given time. Women get TMJ disorder more often than men; in fact, for every male TMJ sufferer, there are 9 female TMJ sufferers.
TMJ disorder tends to be higher among younger people, while women using estrogen or contraceptives tend to experience TMJ disorder more frequently.
What Is TMJ Disorder and What Causes It?
Loosely put, TMJ disorder is any type of pain and restricted movement that impacts the jaw joint and surrounding muscles. There are several different causes of TMJ, including:
- Injury to the tooth or jaw
- Grinding or clenching of the teeth
- Poor posture
- Stress
- Other issues
In some instances, even chewing gum can aggravate an outbreak of TMJ. TMJ disorder can lead to headaches and facial pain.
TMJ Disorder and Headaches
When TMJ sufferers have a headache, they often report a headache that is like a tension headache in nature. TMJ associated headaches often recur in one or more regions of the head and face and are accompanied by several different symptoms:
- Tight face and jaw muscles
- Face or jaw pain
- Clicking noises in the jaw when chewing
- Overall restricted movement of the jaw
- Changes in how the teeth fit together when biting down
It is important to keep in mind that TMJ discomfort can also be a manifestation of migraine headache attacks. Migraines can also cause referred pain to the TMJ areas, neck, shoulders, sinus areas, and face. So if the TMJ discomfort happens primarily when someone has a migraine type headache or symptoms, it could also just be a referred pain syndrome rather than a true TMJ disorder.
Is There a Positive Outlook for TMJ Headaches?
TMJ headaches are incredibly uncomfortable, but there is generally a very good outlook for TMJ headaches. Your doctor may suggest a wide variety of treatments to alleviate the pain and often lifestyle changes and other treatments may be required to eliminate and address TMJ disorder. Treatments aimed at alleviating TMJ disorder itself are generally very successful in reducing the frequency of these types of headaches. Let’s take a look at some of the treatments that are available for TMJ headaches.
Very rarely are TMJ disorders serious and long lasting. In these rare situations, diagnosis and treatment must be sought quickly to manage and resolve the condition. Chronic, severe TMJ disorder is very rare, however, tendons, muscles, and cartilage over time can become damaged leading to arthritis. The good news is that most cases of TMJ disorder go away within about two weeks if the jaw is given the necessary time to rest and the root cause, such as stress, is removed.
Occasionally, TMJ disorder will go away on its own. Self-limiting cases are common and being aware of grinding and clenching can help alleviate TMJ over time if it’s not a severe case.
Lifestyle Changes to Address TMJ Associated Headaches and Facial Pain
Some behaviors may cause and trigger flare ups of TMJ disorder, as well as associated headaches and facial pain. Some people may experience this disorder from the type of food that they eat, the stress in their life, and certain jaw movements that they have learned as habits over the years. Some small lifestyle changes can help with TMJ disorder and associated headaches and pain, including:
- Avoiding foods that are hard or require a great deal of chewing
- Reducing the stress factors in one’s life to prevent jaw clenching and teeth grinding, which are coping behaviors aimed at dealing with stress.
- Learning jaw exercises to strengthen the jaw muscles themselves and avoiding things like gum chewing and wide yawning, which can irritate the jaw joint.
Over-The-Counter Solutions for TMJ Associated Headaches and Facial Pain
For the short-term, certain medications may help alleviate the headaches and facial pain caused by TMJ disorders. These include NSAIDS, such as aspirin, ibuprofen, and naproxen. These can help eliminate a headache as an abortive treatment. Additionally, icing your jaw can also help relieve the pain associated with a TMJ headache. Jaw exercises can help with muscle relaxation and pain symptoms. Muscle relaxers are often prescribed in conjunction with NSAIDs in an attempt to lessen the muscle spasm and clenching of the muscles surrounding the TMJ.
Long-Term Treatments for TMJ Associated Headaches and Facial Pain
There are a wide variety of different treatments for TMJ disorder, which can help relieve headaches and facial pain. These include physical therapy, Botox, surgery, and other types of treatments.
Sometimes, there are certain exercises that may help address TMJ associated headaches and facial pain. Patients can learn various exercises, like chin tucks, upward tongue, forward jaw, and resisted closing movements. These help with TMJ pain relief. Generally speaking, these exercises provide a very good therapeutic outlook for patients.
Some patients may also benefit from alternative treatments like acupuncture and massage. Consulting with a medical professional is advised to make sure that any exercises are learned correctly.
Splints and Mouthguards For TMJ Disorder
Splints and mouthguards are a treatment that may help alleviate TMJ associated pain and headaches. These do not directly treat the pain itself, but can help prevent clenching and grinding of the teeth. Some dentists may fit these for patients after a consultation with a health professional. Seeing a TMJ specialist for these types of treatments is recommended to ensure precision of the device, because if it is off even slightly, the pain can intensify. The idea behind splints and mouthguards are that they prevent the grinding and biting that typically occurs during sleep, allowing the jaw to rest. Sometimes, a dentist will work on a long-term bite placement solution, which is often a frequently successful treatment for TMJ disorder.
Other Treatments for TMJ Disorder and Associated Headaches and Facial Pain
There are other techniques to help with TMJ disorder that are surgical and alternative in nature. A TMJ arthroscopy is a minimally invasive surgery that allows the surgeon to remove inflamed tissue and align the jaw correctly.
Another treatment that may also work is Transcutaneous Electrical Nerve Stimulation. This provides an electrical pulse that creates muscle contractions so that your jaw muscles will massage themselves. This helps relieve pain and stiffness, simultaneously improving your overall jaw mobility.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.
FAQ
TMJ stands for temporomandibular joint. This is a joint that connects your jawbone to your skull and is responsible for helping you chew, speak, and move your mouth. TMJ disorder is caused by a lot of different factors, ranging from trauma, arthritis, an overbite, or wear and tear. TMJ disorder is pain and discomfort that is associated with the movement of this joint. TMJ disorder can sometimes lead to headaches and pain.
TMJ disorder tends to be prevalent among younger people. Women who are using contraceptive devices and estrogen will also be at risk. There is also some data about what types of symptoms people might get based upon their age. According to the NIH, things like stress, family history, demographic, are strong factors in people who have TMJ. One interesting trend is that many people who don’t have a trauma to their jaw have TMJ.
TMJ disorder can cause headaches. According to some research, TMJ disorder is one of the leading causes of headaches. A headache caused by TMJ disorder might be dull, tight, and aching in front of and around the ear, temple, and cheek. Most often, they are on one side of the head. But occasionally they can be on both sides. The clicking and other symptoms that go along with TMJ tend to be related to the severity of the headache and TMJ headaches tend to go away as tension in the jaw is released.
TMJ headaches are a secondary headache, meaning that they are caused by the TMJ disorder. Generally speaking, some of the pain caused by TMJ disorder and the headache can be relieved with NSAIDS, such as ibuprofen. Cold compresses and ice can also be used to relieve pain. Sometimes, things like bite guards can be used to mitigate the symptoms of TMJ disorder and this can help prevent headaches.
Thunderclap headaches are a type of headache where the onset is very rapid, developing in under one minute. They are often characterized as a “first or worst headache” These types of headaches can be a symptom of bleeding in the brain or an aneurysm rupture, requiring immediate evaluation by a doctor. Certain types of strokes can also cause thunderclap headaches. These headaches need to be addressed with emergency care by a qualified physician.
TMJ headaches can last anywhere from a few hours to days or weeks. Undiagnosed TMJ disorder can create headaches that are chronic in nature. Many people who have the disease may not realize it. Undiagnosed TMJ can lead to more debilitating conditions. For example, it can contribute to snoring, sleep apnea, and the amount of oxygen that you breathe in at night. It can also impact how you eat, posture, and your emotions and overall mood.
TMJ headaches can flare up for a wide variety of different reasons. The most common reason is stress. This can lead to teeth clenching, bruxism, and other issues. Eating hard chewy foods will also cause your TMJ to flare up. For women, hormonal changes and birth control can also contribute to TMJ disorder.