
Exploring Effective Options for Chronic Migraine Relief; A Roadmap to Respite
I see patients stuck in the dark lonely rut of chronic migraine all day every day. Chronic migraine is a miserable headache disorder which causes

I see patients stuck in the dark lonely rut of chronic migraine all day every day. Chronic migraine is a miserable headache disorder which causes

Imagine a pain so intense that it feels like a storm raging inside your head, accompanied by a symphony of other symptoms that make even

If you experience headaches every day, you likely have a condition known as chronic daily headache. Generally speaking, the difference between episodic and chronic headaches
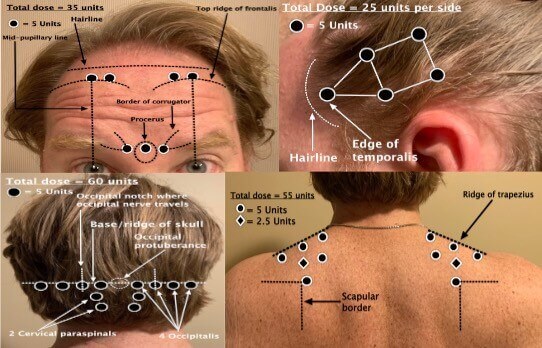
Let’s talk about Botox for migraines. Botox (Onabotulinum Toxin A) has been a game changer for the treatment of chronic migraine. I’ve frequently seen it
I see the worst of the worst headache, migraine, chronic migraine, facial pain, fibromyalgia, and chronic pain from many states and countries. I see patients

Chronic daily headache being endlessly fueled and driven by rebound headache (medication overuse headache or MOH) is one of the most common headache disorders that
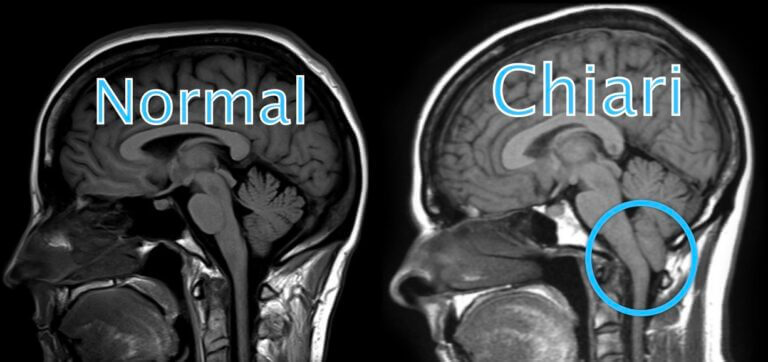
What Is Chiari Malformation? Chiari malformation, also known as Arnold-Chiari malformation, is a common congenital (born with it) condition of anatomical variation involving the brain