Are you one of the millions of people who suffer from migraines? Have you ever considered the impact that your gut health may have on the frequency and severity of your migraine attacks? In this blog post, we will explore the intriguing connection between gut health and migraines, delving into how poor gut health and gut dysbiosis can potentially trigger or worsen migraines. Understanding this relationship and the bidirectional gut-brain axis may provide valuable insights into managing your migraines more effectively.
Introduction to Gut Health and Migraines
To unravel the complex relationship between gut health and migraine headache, it is paramount to understand the dynamic interaction between our digestive system and our brain and central nervous system – an interplay often underestimated in its influence on our well-being. Our digestive tract, populated by trillions of microorganisms including bacteria, viruses, and fungi, forms an ecosystem known as the gut microbiota. In fact, 1-2% of human body weight is bacteria!
This vast microbial community is not merely a passive inhabitant; it plays an instrumental role in our health, neurotransmitter production (90% of our serotonin is made in the gut, mostly by bacteria!), affecting everything from our immune system to our mood and even the likelihood of experiencing migraines.
Disruptions within this microbial community affecting the good bacteria can influence the occurrence and intensity of migraines. This perspective offers a novel approach to understanding migraines, positioning gut health as a significant factor in migraine pathology. The gut microbiota’s influence extends beyond digestion, impacting the regulation of inflammation, the permeability of the intestinal barrier (leaky gut), and the body’s response to pain – all of which are relevant to the migraine experience.
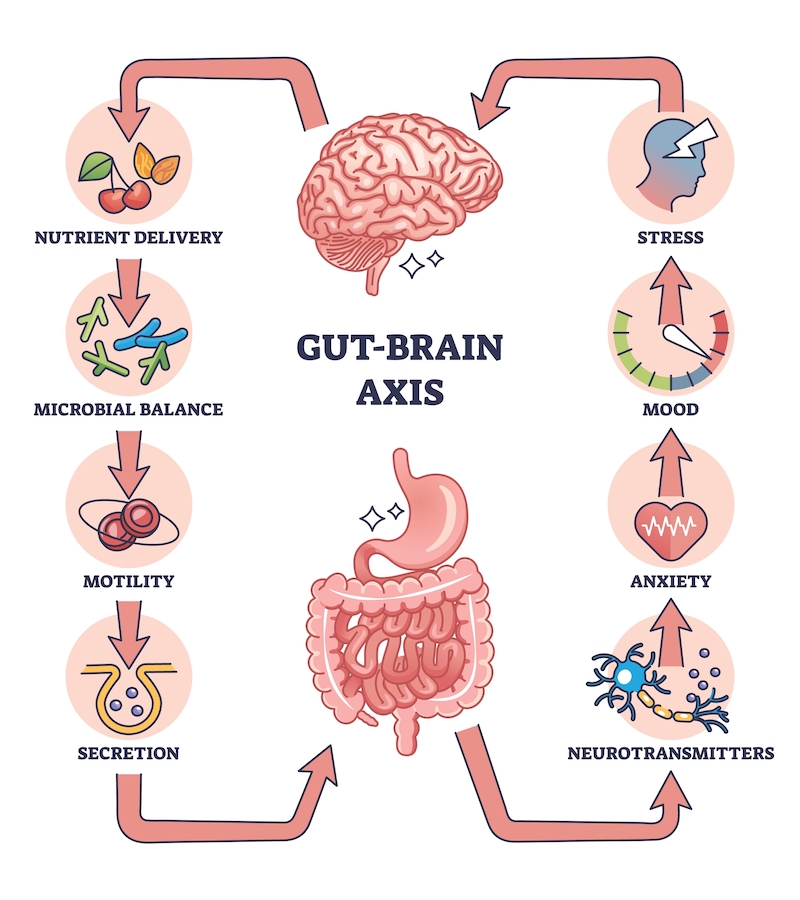
Research has illuminated potential pathways through which gut health can affect migraines, including the modulation of systemic inflammatory responses and the integrity of the gut-brain axis. This bidirectional communication channel between the gut and the brain allows each to influence the other’s functioning, underscoring the complexity of the gut health and migraine connection. By exploring the nuances of this relationship, we open the door to innovative approaches for managing migraines, emphasizing the importance of holistic health practices that support both gut and brain health.
How Gut Health Impacts Migraine Frequency and Severity
Emerging evidence highlights a significant correlation between the state of our gut health and the patterns of our migraine episodes. Individuals grappling with frequent and severe migraines often report concurrent gastrointestinal discomforts, such as bloating, irregular bowel movements such as gastroparesis or diarrhea, GERD (heart-burn or acid reflux) and abdominal pain, suggesting a deeper link between gut disturbances and migraine activities. The presence of conditions like irritable bowel syndrome (IBS), Crohn’s disease, ulcerative colitis, celiac disease, and Helicobacter pylori infection in many migraine sufferers further underscores the gut-migraine connection.
Chronic headache and migraine has been reported in 30% of celiac disease, 23% of irritable bowel syndrome (IBS), and 56% of gluten sensitivity. These gastrointestinal disorders are characterized by an imbalance in the gut’s microbial population and a compromised intestinal barrier—factors that can incite systemic inflammation.
This inflammation is not a localized event; its effects can ripple through the body, reaching the brain and potentially triggering migraines. The inflammatory mediators released can disrupt the delicate balance within the gut-brain axis, exacerbating migraine symptoms. This relationship suggests that interventions aimed at improving gut health could have a direct impact on reducing migraine frequency and severity. By nurturing our gut microbiome and ensuring the integrity of our intestinal barrier, we may be able to alleviate the underlying inflammation that contributes to migraines.
Studies in mice have shown that when their normal gut flora is removed, they develop a higher pain sensitivity at baseline, related to calcitonin gene-related peptide (CGRP) dysfunction. In another study, when the gut flora of mice was removed and transplanted with gut microbiota from migraine patients, the mice developed features of migraine. Similarly, other mice studies showed that removal and sterilization of normal gut microbiota followed by fecal transplant with obese mice or depressed mice led to the mice developing obesity and depression behavior after microbiota transplant, respectively.
Although the precise mechanisms linking gut health with migraines continue to be an area of active research, the existing evidence invites us to consider the health of our digestive system as a critical factor in managing migraine symptoms. Attention to gut health, therefore, emerges not only as a strategy for overall wellness but also as a potential avenue for mitigating the distressing experience of migraines.
The Role of Gut Inflammation in Migraine Development
At the core of understanding how migraines manifest lies the pivotal role of inflammation, particularly within the gut. A normal inflammatory response is a crucial part of the healing process in injured tissues, and part of how the immune system fights infection. However, when inflammation is not regulated properly, too much of a good thing can become bad. Chronic gut inflammation can act as a harbinger for the release of inflammatory mediators that possess the ability to traverse the protective blood-brain barrier, directly influencing the neurological pathways involved in triggering migraine attacks. This occurs via the proposed leaky gut syndrome in which the inflammation causes increased intestinal permeability, allowing toxins, bacteria, or other inflammatory mediators to enter the bloodstream.
This connection between gut inflammation and migraine development is not merely coincidental but is backed by a growing body of research that identifies inflammation as a critical bridge linking gut disturbances to neurological symptoms. It is not uncommon to see someone with chronic inflammatory bowel disease also suffer with chronic migraine.
Addressing this inflammation presents a promising strategy for those seeking relief from migraines. It’s essential to recognize that the foods we consume and our lifestyle choices can either exacerbate or alleviate gut inflammation. An anti-inflammatory diet, rich in whole foods, and devoid of processed options, alongside mindful lifestyle practices, can significantly mitigate the inflammatory responses within the gut. Such measures not only promise to soothe the gut lining but also to reduce the frequency and severity of migraine episodes by dampening the inflammatory signals that reach the brain.
Moreover, the interplay between specific dietary elements and gut health—such as the balance of omega-3 and omega-6 fatty acids, the role of antioxidant-rich foods, and the potential of probiotics to restore gut harmony—highlights the intricate connections that govern our well-being. By fostering a healthier gut environment, we pave the way for a more resilient defense against the triggers of migraine pain, offering hope and a potential path toward lesser reliance on traditional migraine medications. This approach underscores the importance of viewing our bodies as interconnected systems, where gut health is not isolated but deeply entwined with our neurological and overall health.
Understanding the Gut-Brain Axis
The concept of the gut-brain axis underscores the profound and intricate communication network that exists between our digestive system and our brain. The vagus nerve provides a 2 way communication between the brain and the gut. In fact, the vagus nerve sends more signals up from the gut to the brain then it does from the brain down to the rest of the body!
This bi-directional pathway enables signals to be sent from the gut to the brain and back, meaning that changes in our gut’s health can directly influence our neurological state, and vice versa. Conversely, the central nervous system can modulate gut microbiota through the parasympathetic and sympathetic nervous systems and by releasing neuroendocrine peptides. It is a partnership that plays a crucial role in maintaining our overall well-being and is particularly relevant in the context of migraines.
Emerging studies shed light on how disturbances in this axis may have a causal relationship to an increased susceptibility to migraines. For example, an imbalance in gut microbiota can affect the production of certain neurotransmitters such as serotonin, acetylcholine, dopamine, GABA, and CGRP which in turn can influence pain perception and inflammation – both key components in migraine episodes. This point is highlighted by the fact that 90% of the body’s serotonin is made in the gut, mostly by bacteria!
Additionally, the integrity of the gut lining, which when compromised, can allow harmful substances to enter the bloodstream and potentially trigger inflammatory responses that affect the brain, further emphasizes the axis’s significance.
The gut-brain axis also illustrates how psychological stress can impact gut health, leading to a heightened response to migraine triggers. Stress is known to affect gut motility and permeability, which can alter the gut microbiota composition and exacerbate migraine symptoms. This reciprocal relationship highlights the need for approaches that consider both the physical and emotional aspects of well-being in the management of migraines.
In understanding the complexities of the gut-brain axis, we gain valuable insights into the multifaceted nature of migraine headaches. It encourages a holistic view of health, recognizing that the mind and body are inextricably linked, and that nurturing our gut health can have profound implications for our neurological health and general well being.
The Influence of Gut Bacteria on Migraine Symptoms
The complex ecosystem within our gut, teeming with billions of bacteria, has a profound impact on our overall health and notably, on the manifestation of migraines. Scientific exploration into this domain has unveiled that an imbalance in these gut bacteria – a condition known as dysbiosis – may be intricately linked to the prevalence and intensity of migraine attacks, acting as a migraine trigger.
The beneficial bacteria within our gut microbiome play a crucial role in maintaining the delicate balance of our body’s immune response and in modulating inflammation, both of which are closely tied to migraine symptoms. Dysbiosis of gut microbiota has been shown to increase a pro-inflammatory state and increased inflammatory markers in the blood.
This burgeoning field of research posits that the specific composition of one’s gut bacteria could influence the body’s production of certain chemicals and neurotransmitters that are known to play a role in pain perception. For instance, certain strains of gut bacteria can produce precursors or directly synthesize neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), which have the potential to affect the pain pathways involved in migraine attacks, as well as major players in mood. Similarly, some bacteria can influence the level of pro-inflammatory and anti-inflammatory compounds in the body, further affecting migraine susceptibility.
Intriguingly, studies have begun to investigate how supplementation with probiotics – live beneficial bacteria – could restore a healthier balance to the gut microbiota, potentially offering relief to those afflicted by migraines. These supplements aim to counteract dysbiosis, thereby possibly reducing the inflammation and imbalance of neurotransmitters associated with migraine episodes.
As research progresses, the potential of targeting gut bacteria to alleviate migraine symptoms is becoming an increasingly attractive avenue for both scientists and those suffering from migraines. The promise lies in harnessing the power of our gut microbiota to forge a path toward lesser dependence on conventional migraine treatments and toward a future where our gut’s health directly contributes to our relief from migraine symptoms.
Identifying Symptoms of Poor Gut Health
Navigating the signs of compromised gut health can be crucial for those suffering from migraines, as these symptoms may hint at an underlying factor contributing to the frequency and severity of their headaches. Indications of suboptimal gut health are diverse and can range from gastrointestinal discomforts such as persistent bloating, gas, and irregular bowel movements, to gastrointestinal bleeding, to more systemic signs like constant fatigue and unexplained weight changes. These manifestations serve as the body’s signal that the delicate ecosystem within your gut may be out of balance, potentially exacerbating migraine symptoms.
It’s not uncommon for individuals with migraines to notice a parallel between their digestive disturbances and the pattern of their migraine episodes. Such observations underscore the importance of paying close attention to one’s digestive health as part of a comprehensive approach to managing migraines. Keeping a record of dietary habits and corresponding physical responses can be a valuable tool in identifying specific foods or eating patterns that may trigger or worsen both gut and migraine symptoms. This self-awareness empowers sufferers to make informed decisions about their diet and lifestyle, paving the way toward mitigating the impact of migraines on their lives.
Recognizing and addressing symptoms of poor gut health demands a mindful and proactive approach. By acknowledging these signs, individuals can take the first step towards restoring their gut balance, potentially reducing the intensity of their migraine experiences and enhancing their overall quality of life.
Diet and Lifestyle Changes to Improve Gut Health
Embracing a holistic approach towards nurturing your gut health can pave the way for significant improvements in both digestive well-being and migraine management. Initiating changes that foster a vibrant and balanced gut microbiome involves incorporating a variety of nutrient-dense foods. Prioritize the intake of prebiotic-rich foods, such as bananas, oats, barley, green onions, apples, cocoa, garlic, onions, and asparagus, which fuel and feed the beneficial bacteria in your gut. Think of prebiobiotics as food for the microbiota. If you want healthy gut bacteria, you must feed them healthy food.
Simultaneously, integrating probiotic foods like yogurt, apple cider vinegar, olives, kefir, kimchi, pickles fermented cheese, and sauerkraut into your diet can introduce beneficial strains of bacteria, bolstering your microbiome’s diversity and resilience. Think of probiotics as ingesting live healthy bacteria micro-organisms to transplant into your gut’s ecosystem. Probiotic supplements containing multi-species and multi-billion counts of bacteria can also be added to diet. Some patients even undergo fecal microbiota transplant (FMT) if they are having a hard time improving their gut health.
Equally important is the reduction of inflammatory foods that can disrupt gut health and potentially exacerbate migraine symptoms. Processed foods, high-sugar snacks, and foods containing artificial additives should be limited. Opt instead for whole, unprocessed foods that are naturally rich in antioxidants and omega-3 fatty acids, which support the reduction of inflammation.
Benefits of optimizing the gut microbiome can include improved intestinal mobility and permeability, improved gut and systemic immune responses, and intestinal cellular lining integrity.
Lifestyle adjustments and environmental factors play a crucial role as well. Regular physical activity, even mild to moderate exercise, can enhance gut motility and microbiome diversity. Keeping hydrated is very important. Managing stress through mindfulness practices, meditation, or yoga can also mitigate the adverse effects of stress on gut health, contributing to a more harmonious gut-brain axis.
The Potential Benefits of Probiotics for Migraine Relief
Exploring the arena of probiotics reveals a promising frontier in the quest for migraine relief. These beneficial live bacteria, when ingested in the right quantities, are known to foster a healthy gut environment, potentially easing the symptoms associated with migraines. The science behind probiotics suggests that by rebalancing the gut microbiota, these microorganisms can play a pivotal role in modulating the body’s inflammatory responses — a key factor in the onset and severity of migraine episodes.
Delving deeper, fine-tuning which probiotic strains to use might influence the production of neurotransmitters and inflammatory mediators, thereby impacting migraine pathology. For individuals navigating the challenges of frequent migraines, incorporating probiotics could represent a beacon of hope. It is, however, essential to approach this potential solution with mindfulness and informed discretion.
The diversity of probiotic supplements available today underscores the importance of selecting a product that aligns with one’s unique health profile. Engaging in a dialogue with a healthcare professional can help pinpoint the probiotic supplement strains that might offer the most benefit, tailoring the approach to one’s specific needs. This personalized strategy underscores the complexity of migraines and the nuanced role gut health plays in mitigating their impact, highlighting the innovative avenues being explored in migraine management and relief.
Reducing Inflammation Through Diet and Supplements
Adopting an anti-inflammatory diet emerges as a pivotal strategy in the battle against migraines, with a focus on consuming foods that naturally quell inflammation within the body. Central to this approach is the inclusion of a wide array of fruits and vegetables, which are laden with antioxidants and phytochemicals, substances known for their ability to reduce oxidative stress and inflammation. Healthy fats, particularly those found in avocados, nuts, and seeds, along with omega-3-rich fish such as salmon and mackerel, are also cornerstone components of an anti-inflammatory diet. These foods not only support brain health but also contribute to the maintenance of a balanced immune response, which can mitigate migraine triggers.
In tandem with dietary adjustments, the strategic use of supplements can bolster your body’s defenses against inflammation. Omega-3 fatty acids, available in fish oil or algae-based supplements, stand out for their potent anti-inflammatory properties. Turmeric, a spice celebrated for its curcumin content, offers another powerful tool in moderating inflammatory processes in the body. Magnesium, a mineral with multiple health benefits, has been specifically linked to improvements in migraine frequency and intensity by several studies. Incorporating these supplements, under the guidance of a healthcare provider, can enhance the effectiveness of dietary changes, creating a comprehensive strategy for managing migraine-related inflammation.
The Importance of Professional Medical Advice
As we navigate the complexities of intertwining gut health with migraine management, it becomes increasingly clear that professional oversight is mandatory. The insights provided here serve as a springboard for understanding potential strategies that may alleviate migraine symptoms through gut health optimization. However, each individual’s experience with migraines is as unique as their gut microbiome, underscoring the necessity for tailored medical advice.
Engaging with a healthcare provider ensures that any adjustments to your diet, lifestyle, or supplement regimen are not only conducive to enhancing gut health but are also aligned with your specific health needs and migraine management plan. In addition, if you are having any gastrointestinal symptoms such as abdominal discomfort, nausea, vomiting, diarrhea, blood in the stool, bloating, or anything else, excluding underlying gastrointestinal diseases is crucial. This personalized approach facilitates a safer and more effective journey towards managing migraine symptoms, reminding us of the invaluable role that professional medical guidance plays in our overall health strategy.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.