Botox for Migraines
Botox for migraine headaches? This is often the response along with a confused look on a patient’s face when I discuss and recommend Botox injections for migraines, and specifically chronic migraine. So let’s talk about Botox shots for migraines. This blog will discuss how Botox works, and what you need to know about Botox treatments. It will show you exactly where to inject Botox for migraine headaches.
As you’ll see, the Botox for migraines injection sites precisely target a large number of nerves that travel throughout the face, head, scalp, neck, and shoulders. Ultimately, the way that Botox works for chronic migraine is to disrupt the electrical pain and headache signals traveling through those nerves and pain pathways. Botox also causes muscular relaxation, which can also provide pain relief.
Patients and healthcare providers often ask me, “where do injections of Botox go for migraines”? So this blog will show you where it goes and what to expect. It will also provide the education and guidance in optimizing the Botox procedure technique for medical providers to give precision treatments resulting in better results. Feel free to share this pattern and blog with your doctor if they do not do a lot of Botox (or if you are not getting a good response!).
What is Botox for Chronic Migraine?
Botox (Onabotulinum Toxin A, or botulinum toxin type A) has been a game changer for the treatment of chronic migraine headache pain. I’ve frequently seen it give people their life back by restoring their ability to function normally in daily activities and many aspects of life, helping to pull them from the dark rut of chronic migraine that people get stuck in. It can assist in stopping medication overuse headache (rebound headache), which often contributes to chronic migraine. Once Botox is working, patients can often wean off daily pills being used for migraine prevention.
Botox is a neurotoxin made by the Clostridium botulinum bacteria. I know that sounds scary and weird, but this toxin is incredibly medicinal when used properly. When ingested, it is the same toxin that causes botulism, a form of food poisoning. Yes, this idea freaks many patients out. However, the amount used for chronic migraine is a much lower potency and dose, and when used correctly, can be an amazingly helpful medication.
Botox is produced by AbbVie, and was FDA approved for the treatment of CHRONIC migraine in October 2010 following this study. Since 2010, it has technically remained the only truly FDA-approved treatment specifically indicated for the treatment of chronic migraine prevention, up until Qulipta (Atogepant) became the first and only pill to receive FDA approval for chronic migraine in 2023. With that said, the array of standard preventive migraine treatments as well as the CGRP monoclonal antibodies are also commonly used for all spectrum of migraine from episodic migraine (14 or less headache days per month) to chronic migraine (15 or more headache days per month).
How Does Botox Work For Chronic Migraine?
The primary and most important mechanism of how Botox works for chronic migraine is by disrupting the electrical communication signals of pain between nerves involved in migraine pathophysiology and ultimately stopping these signals from reaching the pain circuitry of the brain. Thus, it prevents the activation of pain and migraine networks in the brain, including disruption of CGRP activity, which has become a central focus in most of the new migraine medications on the market such as the gepants and CGRP monoclonal antibodies.
Botox does this by entering the nerve endings and cleaving a specific protein called SNAP25. The inactivation of this protein leads to the inhibition (stopping) of neurotransmitter and neuropeptide release from the nerve endings and the prevention of the electrical pain signals from firing off. It also causes temporary (3 months) paralysis of the muscle being innervated by those nerve endings. Thus, it also causes the muscles to chemically relax (by chemically paralyzing them). For example, this muscle relaxation is why Botox works for facial wrinkles. It causes the thin muscular layers to relax to where they can’t contract (and wrinkle the skin), and wrinkles go away. Interestingly, one of the early clues that led to Botox being studied for migraine treatment was that women who were getting cosmetic Botox were also noticing that they would have many less migraines. This led to trials looking at Botox treatment to prevent migraine, which it was confirmed to do.
How Long Does It Take For Botox To Work? How Long Should Botox Be Used For Chronic Migraine? How Effective Is Botox?
Injections of botulinum toxin (Botox) typically starts to take effect within 1-2 weeks, but many patients say they feel it working within a couple days. Some patients report relief immediately after injections, which I believe may be an acupuncture-like effect that some may be responsive to.
Botox lasts about 3 months. So it is a simple treatment done only 4 times per year. Patients commonly notice some gradually increasing migraines 1-2 weeks or so before getting to the 3-month wear-off window. Some can consistently get a good 4 months out of a treatment, but that is not common. If patients consistently start to come in for their 3-month Botox appointment and migraines are not starting to increase significantly as it is wearing off, I will often try to extend the next treatment to 4 months. If they are still doing well at 4 months, I suggest that we try stopping it to see if the migraines have entered into a more stable episodic pattern. It can always be restarted if needed in the future.
Some people wear off by 8-10 weeks, so some receive Botox every 10 weeks. However, it is best to avoid treatments consistently under 12 weeks when possible because there may be some risk of antibody formation against Botox which can make it less effective over time. If done too early, there can also be overlap of doses which may increase potential for side effects if the prior round hasn’t fully worn off yet.
It is recommended to give the Botox a minimum of 2 rounds 3 months apart to get a good sense of how much benefit one can likely expect. The reason is because after the 2nd round, there is often additional improvement noted. With that said, I typically expect (and usually see) good improvement with the 1st round. If there is no improvement with the 1st round, the recommendation is still to do the 2nd round because many times it may start working then. Some doctors advocate for giving a full year (4 rounds separated by 3-month intervals) to see the full effect. However, I typically tell patients if they have gotten absolutely no benefit after the 2nd round that we should move on to another treatment option. On average, in the main trial, Botox decreased chronic migraine days by 8-9 days per month, as opposed to placebo which was 6-7 days per month.
What Are Botox Side Effects?
A great thing about Botox for treatment of migraines is that it is so well tolerated with much lower side effect risks compared to many of the medications used for migraine prevention. I’ve done thousands of Botox treatments and have never seen someone have a bad reaction or an allergic reaction. That doesn’t mean it’s not possible though.
So what are the common side effects of Botox? In general, I tell patients there may be some tenderness in the injection sites temporarily. It is a very tiny needle injected just under the skin in a specific standardized dosing pattern and takes only a few minutes. Infrequently, patients can have a temporary flu-like muscle achiness for a day or so after the Botox. If the Botox spreads into some of the muscles in the forehead, I always mention that there is a risk of eye lid droopiness (ptosis), although I have not seen this occur personally. There are rare reports of trouble swallowing, breathing, or neck weakness, and these could relate to faulty technique or excess dosing. However, these are not things that we really see in the headache world with the doses and locations that we use for chronic migraine. A more extensive list of potential side effect risks (which are very rare), can be read on the Botox for chronic migraine AbbVie website. Caution is also advised if Botox is mixed with bupivacaine or other “caine” medications as this can be a fairly common allergy of some patients to these medications.
There are some medical conditions in which Botox should be avoided. If you have a significant neuromuscular disease such as myasthenia gravis, Lambert-Eaton Syndrome, or amyotrophic lateral sclerosis (ALS), you should avoid Botox. Botox should never be administered in an area of skin infection. Caution is advised in those with severe respiratory or pulmonary diseases, especially in those with chronic oxygen tank dependence.
Is Botox Safe In Breastfeeding And Pregnancy?
Historically, Botox has generally been avoided and saved as a last resort option in these scenarios, but times are changing. The longstanding concern for using Botox during breastfeeding is based in theoretical concern that the Botox could seep into the breastmilk and affect the baby, although this really hasn’t been reported.
It has been shown that Botox is not detectable in the blood after intramuscular use, so excretion into breast milk is considered unlikely. In fact, there was a published case of a lactating woman who had food borne botulism (exponentially higher amount of toxin load than what is received during a Botox treatment). However, when the breastmilk and infant were analyzed, neither showed any botulinum toxin at all, and the infant was safely breastfed. With this in mind, the doses of Botox used medically are much lower than those that cause botulism. So it is felt to be extremely unlikely that Botox will enter the milk. Therefore, the risk of Botox during breastfeeding is felt to be very low, and most headache specialists perform Botox during breastfeeding now given the overall data and clinical experience collected over the years.
Regardless, for extra precaution, some recommend breastfeeding before the Botox treatment along with storing some milk, and then pump and dump any milk produced in the subsequent 12 hours after Botox (so plenty of milk should be saved ahead of time). These recommendations are not an absolute and are variable between different doctors, but it is a consideration for those who are still worried.
Similar to breastfeeding, the use of Botox during pregnancy has become more widely accepted and practiced by most headache specialists given the years of data published and clinical experience. Since Botox is not detectable in the blood after intramuscular use it is not expected to affect fertility or pregnancy outcomes, and a safety database report has remained consistent with this conclusion. Botox is designated as a US Food and Drug Administration (FDA) pregnancy category C medicine, meaning that there are no well controlled studies in pregnant women, so it should only be used during pregnancy if the benefits outweigh the potential risks, which is typically the sentiment nowadays.
What Is The Injection Pattern for Botox For Migraines?
If you are going to get Botox, you need to make sure you are getting the optimal dose, pattern, and technique with someone that does A LOT of Botox and is very experienced. I can’t tell you how many times a patient tells me they had Botox in the past and it didn’t work with other physicians, nurse practitioners or physician’s assistants. However, when I have them describe the pattern they received, or look at the procedure note, it is almost always a suboptimal pattern and/or dose. Or they describe it as being done very quickly, with deep injections, overly painful injections, or Botox running down the face. These are signs of a probable lower quality treatment. Not surprisingly, when I do their Botox they often respond very well (and they usually tell me it was much different than what they received in the past), and almost always they mention that it was significantly less painful.
There are so many very subtle technique enhancements that lead to a better treatment response and experience. Therefore, I can’t emphasize the importance of an experienced injector enough. I have some patients that fly in for a quick Botox appointment every 3 months because they can clearly see how important this point is given their past experiences with many other injectors.
A headache specialist will have the most refined technique and experience doing Botox injections, and should be sought out to ensure you are getting the best technique if one is available near you. If you cannot find a headache specialist near you, make sure whomever you get the Botox injections from does them very frequently with good reviews. Other doctors that may do Botox injections as alternatives if a headache specialist is not available include some neurologists and pain management doctors. However, most of the time when I see Botox done with general neurology or pain management, the techniques and patterns are not adequate, and the patients often don’t respond.
Don’t even consider getting Botox for chronic migraine at your friend’s “Botox party”. These are not typically physicians, but rather nurses, physician’s assistants or nurse practitioners, and I can assure you that you will not receive a proper treatment, even if it is some type of physician.
Ok, so you want to know where to get Botox to stop migraines? This is a very common question I get. The pattern that should be used and modeled after is the PREEMPT protocol (Phase III REsearch Evaluating Migraine Prophylaxis Therapy), based off the trial that led to FDA approval for Botox in the prevention of chronic migraine.
The pattern of injections described and illustrated below are of the same PREEMPT protocol. However, sometimes I tweak some of the injection sites depending on the patient’s pain pattern. For example, if their chronic migraine is 100% one sided, I may give additional on that side of the head, taken from the opposite side where they have no or minimal pain. If they have prominent occipital neuralgia, then I will give additional dosing over the correlating occipital nerves (I do this very commonly is most patients I treat).
Another common question is how many shots do you get with Botox for migraines? In general, there is a minimum of 31 injection spots for the basic standard Botox treatment pattern for chronic migraine. Each injection is typically 5 units of Botox. I personally do a more specialized pattern involving about 41 injection spots (shown below, but there can be variation) which includes the basic pattern, with additional precision targeting, and a what I typically see as a more effective dose.
The PREEMPT protocol in the clinical trials evaluated 155-195 units of Botox. Botox vials come in 100 or 200 unit vials. For almost all patients, I use the full 200 units. Honestly, I feel the 155 units that many people give is just way too low to get the best effect usually seen with the full 195-200 unit dose. I may use slightly less in patients that have no pain at all in many areas of the head or shoulders and have a very localized pain (such as just in one side of the forehead), are elderly, or young in late teens or early twenties and have not had it before.
For many of the spots the patient receives injections in according to the injection paradigm, they may not have much headache or pain at baseline. However, there should still be some degree of symmetry for muscle weakness balance and to still hit potential areas of chronic migraine input that aren’t recognized as overly painful areas by the patient. I also personally gently rub in the Botox spots right after injection. This helps to distract the brain from the immediate injection pain, flattens the area so it doesn’t leave the Botox as a small lump, and helps to slightly spread the area of coverage for the Botox to work. I like to hit as many of those sensory nerve fibers (the primary target of Botox for chronic migraine) and neuromuscular junctions as possible with each injection.
The depth of injection isn’t supposed to be deep. So if the needle is hitting the bone, it is too deep and will be less effective. The target of the injections for chronic migraine is just below the skin and above the muscle layer. This is where the sensory nerves travel (carrying migraine/headache/pain signals to the brain) and neuromuscular junctions lie (where the nerves that innervate and control the muscles enter the muscle). These sensory nerves traveling just above the muscular layer is really the main target of the Botox for chronic migraine.
So, I like to be strategic where the Botox goes. If your doctor or health care provider is just rapid firing it in (which is always more painful), hitting the bone, you have Botox running down your face, it is more painful than when you get it done with other providers, or you get eye-lid droopiness (ptosis), you should think about moving on to someone with a more refined technique. I see patients all the time that have been getting Botox with me and then they have to get a round sometimes with a different provider for some reason. They invariably say it doesn’t work as well, is significantly more painful, and afterwards they refuse to get Botox with anyone else besides me following that experience. There is validity in that. I’ve spoken to one of the primary doctors/researchers involved with developing the original Botox pattern, technique, and dosing for chronic migraine and he agreed that technique and spreading the Botox around strategically and precisely will certainly lead to a better result as opposed to just quickly and less carefully “throwing the injections in”. In fact, they were originally thinking of adding more spots to further spread the Botox around to hit more nerve endings, but they settled on the current pattern to make it easier and less complex to do.
The Botox trials were done by mixing Botox in 0.9% normal saline (basically, sterile water). However, I will sometimes mix the Botox instead with a numbing medicine such as bupivacaine or ropivacaine. The Botox typically takes about 1-2 weeks to start kicking in, but the addition of a numbing medicine can provide some temporary relief as the Botox is slowly kicking in. Many times chronic migraine patients are significantly tender throughout their head to the point the hair can “hurt” and feel sore. This is called allodynia, or central sensitization, and is a common finding in chronic migraine. The additional numbing medicine can also provide some temporary relief throughout some of these sore areas. In most patients, they have tenderness over their occipital nerves in the back of the head (occipital neuralgia), and this can also provide some additional temporary relief over these nerves. Many chronic migraine patients also have tenderness throughout their shoulders, and many have associated fibromyalgia. This can also be helpful with some temporary relief through these muscles, and in a way is like getting trigger point injections at the same time.
So, let’s go over the treatment pattern that I have seen to be most useful. First, you will need to get the supplies together, of course. For doctors and health care providers who are here to learn how to do Botox or fine-tune their skills, a detailed video of what you need and how to draw up the Botox can be seen here. I won’t go through the detailed steps here in mixing and drawing the Botox up, but in short, you will need:
-Botox 200 units (100 unit vials x 2 vs. a single 200 unit vial)
-1 cc syringes x 4
-3 cc syringe x 1 (to draw up diluent and mix in Botox vial)
-30 gauge ½ inch needles x 4 (to place on end of 1 cc syringes prior to injections)
-18-22 gauge needle x 1 (to place on end of 3 cc syringe to draw up diluent and mix in Botox vial)
-0.9% normal saline vial x 1 (alternatively can consider 0.25% bupivacaine or similar)
-Alcohol pads
-Gauze pads
With knowledge of the precise pattern and technique as outlined below, and enough practice, anyone should be able to do Botox procedures proficiently in the office. It is an easy procedure and can provide dramatic improvement in chronic migraine pain and disability.
Where do neurologists put Botox for migraines?
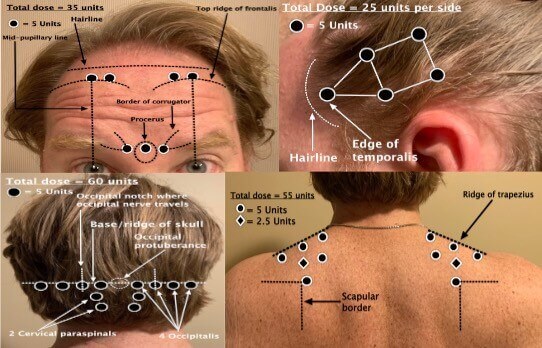
The Botox procedure: Face and frontal regions of head (frontalis and corrugator muscles)
For these injections, I prefer to have the patient lying supine on their back and I stand at the head of the exam table behind them. That way they don’t see the needle coming towards their face and all spots are easily accessed from the top and sides of the patient. These spots are pretty standard in all patients. The things to keep in mind are not doing the Botox too low in the forehead. This can cause ptosis, eyelid droop, and asymmetric eyebrow pointing (think Joker in Batman). I typically inject somewhere just below the hair line and in the very top edge portion of the frontalis muscles or just above it. The first frontalis muscle injection is identified as drawing an imaginary line from mid-pupil up to the top of the frontalis muscle and injecting there. The second is in a horizontal line about a half inch medial to the first injection on each side. The procerus is injected at approximately the middle of the brow right between the eyebrows. The corrugators are injected just lateral to each side of this central injection, about a half inch to each side. All injection sites are 5 units.
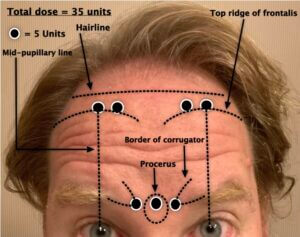
The Botox Procedure: Side Of Head (Temporalis Muscles)
For these injections, the positioning is the same as above. The way that I teach our headache fellows and other staff to do the temporalis muscles are to have the patient clench their jaw and feel for the temporalis muscle to contract. This is felt at the anterior point of the muscle just behind the hair line in the temple region. This is the first injection. From here, imagine a triangle with this first injection as the first point in the triangle. Then draw an imaginary triangle from here extending further back on the side of the head with the next 2 injection points above and below (see illustration) this first point. Then from here, imagine a square connected to the triangle. The next 2 injection points are horizontal and further back from the prior 2 injections points. All injection sites are 5 units.
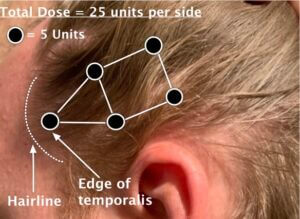
The Botox Procedure: Back Of Your Head (Cervical Paraspinal And Occipitalis Muscles)
For these injections, I prefer to have the patient sitting up on the side of the exam table with their legs hanging over. I stand on the opposite side of the exam table behind them. The cervical paraspinal muscles are injected first on each side. The first cervical injection site is located by feeling the occipital protuberance (bump in the middle along the skull base), and going 2 finger breadths down and 1 over. This happens to be where the greater occipital nerve pierces through the musculature, and is also the first site of where occipital nerve blocks are usually done. The second cervical injection site is located just superior and lateral to the first injection site.
Next come the 4 occipitalis muscle injections. These are done along the skull base and are evenly spaced out. The first site is just lateral to the occipital protuberance. The second site is lateral to the first over the occipital groove (this is a palpable groove). This is where the occipital nerve travels alongside the occipital artery, and is also the second site where occipital nerve blocks are normally done. Withdraw the syringe at this spot to ensure no blood flow given that the occipital artery travels here. The third site is lateral to the second site. The fourth site is lateral to the third site and is located just posterior to the mastoid bone in another palpable groove. This is where the lesser occipital nerve travels, and it also happens to be the third spot normally done for an occipital nerve block.
If the patient has prominent occipital neuralgia on one or both sides, instead of the standard 5 units over the occipital groove region (where the occipital nerves travel), I inject 10 units at once and take that extra dose away from the shoulder or temporalis muscle regions (depending on where they typically have the least amount of pain and may not need it as much). Otherwise, all injection sites are normally 5 units. Notice that the PREEMPT protocol does not include Botox injections further down through the neck. The reason is because this can often increase headaches and can cause neck weakness and head drop to the point where some patients may need to wear a soft collar for 3 months. Therefore, this area should be avoided.
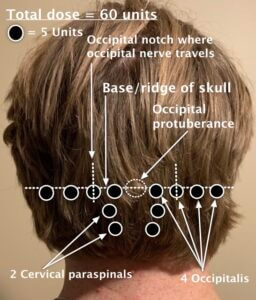
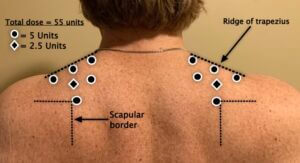
The Botox Procedure: Shoulders (Trapezius Muscles)
For these injections, the positioning is the same as above. Patients with chronic migraine most often have a lot of neck and shoulder pain. 70% of patients that get a migraine will get neck pain and muscle tightness in these regions. So, if they are stuck in a smoldering cycle of chronic migraine and high frequency headaches, they usually have a lot pain, tightness, and muscle contractions in these areas. Many patients also have concurrent fibromyalgia, so these injections can also be helpful, similar to trigger point injections.
The first 3 injections are along the top ridge of the trapezius muscle. If you feel the superior medial corner of the scapula, there is invariably a tender point and knot here. This is the fourth injection site. The fifth site is in the middle of the trapezius muscle bulk. The last 5 units that are left over I typically split between sides by giving 2.5 units somewhere in the trapezius region on each side where there may be a tender or trigger point, or I’ll just give it all on one side if they have more spasm or pain on one side compared to the other.
Does Insurance Cover Botox? How Much Does Botox for Chronic Migraine Cost?
At this point, most insurance plans cover Botox, including Medicare and Medicaid. Many insurances may still require a failure of at least 2 categories of standard preventive medications before they will approve Botox coverage, but these requirements are starting to loosen up. In addition, AbbVie provides a Botox Savings Program which will cover $1000 of any out of pocket costs per treatment and $4000 per year. So for most patients, Botox treatments can be covered 100% between this savings program and insurance coverage.
Conclusions
Botox for the treatment and prevention of chronic migraine has been a game changer for many patients. It is a simple treatment done 4 times per year (every 3 months). Once Botox starts working, many times preventive medicines can be weaned off and stopped. The key to an effective treatment and a good experience is having an experienced headache specialist (preferably) who does a lot of Botox to ensure you are getting a fine tuned technique and injection strategy, based on your personal pain patterns and examination.
Botox often provides a significant improvement in quality of life with low risk of serious side effects. If you continue to have chronic migraine, are not responding to or tolerating standard preventive treatments, discuss Botox with your healthcare provider to help lessen the frequency and severity of your migraine attacks and migraine symptoms.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.