Imagine feeling a migraine coming on without any of the usual pain. That’s what acephalgic migraine is like. These mysterious headaches can cause light sensitivity, nausea, and other symptoms—without the throbbing head pain that typically signals a migraine attack. While they may sound like a dream come true for those who suffer from painful migraines, acephalgic migraines can still be disruptive to everyday life and should be taken seriously by sufferers. Read on to learn more about this strange condition and how it is treated.
Understanding Acephalgic Migraine
Acephalgic migraines, also known as silent migraines or migraine aura without headache, are a type of migraine characterized by visual disturbances, nausea and sensitivity to light without any head pain. It is considered a “migraine variant”. They can last minutes to hours and may even be mistaken for a seizure or stroke. The most common symptom of an acephalgic migraine is called an Acephalgic Migraine aura, which typically consists of visual changes such as zig-zag lines and flashes of light.
Other symptoms may include nausea, dizziness, fatigue and difficulty concentrating. While the pain associated with a regular migraine can be debilitating, acephalgic migraines often go undiagnosed or untreated because the lack of pain may make them seem less severe. However, it is essential to seek medical attention if you are experiencing an acephalgic migraine, as these visual disturbances can still disrupt daily life.
Acephalgic Migraine Symptoms: What to Look Out For
The symptoms of an acephalgic migraine can vary from person to person but usually include one or more of the following:
Visual Disturbances
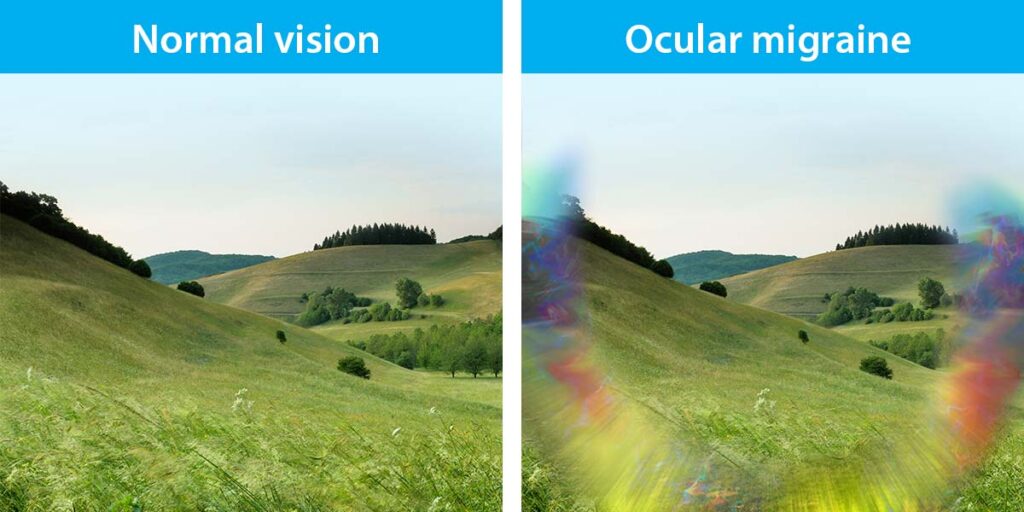
These can range from light flashes or zig-zag lines, colors, prizms, shapes, to a temporary blind spot or even an entire field of vision that is blocked out.
Blind Spots: How Acephalgic Migraine Affects Your Vision
Acephalgic migraines can significantly impact your vision, even without the typical head pain associated with regular migraines. The most common symptom of an acephalgic migraine is called an Acephalgic Migraine aura, which typically consists of visual changes such as zig-zag lines and flashes of light. These disturbances in vision can range from light flashes or zig-zag lines to a temporary blind spot or even an entire field of vision that is blocked out.
These symptoms are caused by a spreading wave of electrical activity across the cortex (outside) of the brain moving at about 2-3 mm per minute. As it spreads across the visual cortex, these visual symptoms are triggered as the neurons are activated from this electrical wave.
This disruption to one’s vision can be incredibly disorienting and may lead to difficulty concentrating or performing daily tasks until the symptoms dissipate. While physical pain does not usually accompany these visual disturbances, they should still be taken seriously as they can significantly affect day-to-day life.
Sensory Changes
Sensory changes are another common symptom of acephalgic migraines that can significantly disrupt a person’s day-to-day life. These sensory disturbances may include tingling sensations, numbness, or an altered sense of smell, taste or touch. Similar to the mechanism of the visual aura described above, if this electrical wave spreads across the sensory cortex, these symptoms become evident.
While these symptoms are not accompanied by the typical head pain associated with regular migraines, they should still be taken seriously, as they can affect one’s ability to perform daily tasks until the symptoms dissipate.
Speech Difficulties
In some cases, an acephalgic migraine may cause speech difficulties. This can range from stuttering or difficulty forming words to a prolonged lack of speech in extreme cases. Similar to the mechanism of the visual aura described above, if this electrical wave spreads across the speech cortex, these symptoms become evident. It is essential to seek medical help if you are experiencing this symptom, as it can disrupt day-to-day life.
Motor Weakness
Motor weakness can sometimes occur in conjunction with an acephalgic migraine. This may include difficulty coordinating movements, walking or maintaining balance. Similar to the mechanism of the visual aura described above, if this electrical wave spreads across the motor cortex, these symptoms become evident. It is important to seek medical help if you are experiencing this symptom, as it can disrupt daily life until the symptoms dissipate.
Other Possible Symptoms of Acephalgic Migraines
Along with the above symptoms, other possible signs of an acephalgic migraine include:
- Nausea
- Dizziness
- Fatigue
- Difficulty concentrating
It is important to remember that the symptoms of acephalgic migraines can vary from person to person and even among different episodes. If you think you may be experiencing an acephalgic migraine, it is essential to seek medical attention, as these visual disturbances can still be disruptive to daily life. Knowing the signs and symptoms can help you recognize when it’s time to seek medical help and get the needed treatment.
It is important to rule out stroke and more concerning causes of any of these symptoms before assuming your symptoms might be migrainous, and this goes for any of the symptoms discussed above. In addition, migraine aura symptoms should last between 5-60 minutes. If they are lasting longer than this, you need to seek further medical evaluation and treatment.
Acephalgic Migraine Triggers: What You Need to Know
If you want to overcome your ailment and continue with your life, you must know the triggers and what to do about them.
Stress and Anxiety
Stress and anxiety are two of the primary triggers for acephalgic migraines. It is vital to have a good understanding of the triggers and what to do about them to manage your symptoms. Mindfulness Meditation, Yoga, Relaxation Techniques, and Cognitive Behavioral Therapy (CBT) can all be beneficial in managing stress and anxiety levels.
Hormonal Changes
Hormonal changes such as those experienced during the menstrual cycle can also trigger acephalgic migraines. Understanding your body’s hormonal cycles and taking steps to manage them can help to reduce your symptoms. This may include tracking ovulation cycles, limiting caffeine intake, avoiding certain foods, exercising regularly, and getting adequate sleep.
Certain Foods and Beverages
Your diet can also play a role in your acephalgic migraine symptoms, and there are many dietary triggers to be aware of. It is essential to ensure that you eat a balanced diet with plenty of fruits, vegetables, lean proteins, and healthy fats. Eating regular meals throughout the day can also help to manage your migraines.
Environmental Triggers
Environmental factors such as changes in weather, bright lights, smoke, or strong smells can also trigger acephalgic migraines. Being aware of your surroundings and limiting exposure to triggering environments may help reduce the frequency and intensity of your episodes.
Other Possible Triggers
Other possible triggers for acephalgic migraines include atypical levels of exercise, certain medications, insufficient sleep, and changes in your daily routine. It is important to be aware of all the potential triggers so that you can take steps to manage them and reduce your episodes.
Acephalgic Migraine Treatment: Options and Strategies
Here are some treatment options and strategies if you suffer from Acephalgic Migraines.
Medications
Medication is often the first line of defense for those suffering from acephalgic migraines. Various medications are available to help manage symptoms. However, since there is no pain with acephalgic migraine, the standard abortive options such as triptans, gepants, nonsteroidal anti-inflammatory drugs (NSAIDs), and anti-nausea medications are of little use. Migraine prevention treatments to try to lessen the attacks from happening is really the most important strategy for this type of migraine variant.
Each medication works differently to target specific symptoms associated with acephalgic migraines, so it is important to speak with your doctor about which option may be best for you. Keep in mind that there are really no good abortive (acute) medicines that help to abort aura symptoms. These are more helpful if there is some level of associated headache with the attacks. Otherwise, if the episodes are frequent enough, the focus is on migraine prevention treatments to try to lessen the attacks from happening.
Can Over-the-Counter Painkillers Help Alleviate Symptoms?
Before self-medicating with over-the-counter painkillers, discussing each type’s possible side effects with your doctor is important. Some common OTC painkillers can effectively manage the pain of migraine, but will do little for the non-pain symptoms of acephalgic migraines. Long-term use is not be advisable as they can cause other health issues.
Lifestyle Changes
Acephalgic migraines can be difficult to manage, but there are lifestyle changes that may help reduce the frequency and intensity of your episodes. Regular exercise, sleep hygiene practices, and dietary modifications can all play a role in managing your symptoms.
Alternative Therapies
Traditional medications may not be enough for those suffering from acephalgic migraines to manage their symptoms. Fortunately, there are a variety of alternative therapies that can help treat the condition and provide relief from the pain and other associated symptoms.
Acupuncture, chiropractic care, massage therapy and biofeedback are some treatments available for individuals struggling with acephalgic migraines. Magnesium and Vitamin B2 (Riboflavin) are two supplements that can often be helpful in helping to prevent aura symptoms, as well as migraine attacks.
Complementary Treatments
Complementary treatments such as yoga, meditation, hypnosis, and mindfulness can also benefit individuals with acephalgic migraines. These techniques can help reduce stress levels, which can trigger the condition.
Other Possible Strategies
In addition to medications and alternative therapies, other strategies may help reduce the frequency and intensity of your episodes. These include avoiding common triggers such as certain foods, alcohol, caffeine, and environmental factors; maintaining a balanced diet; managing stress levels; and getting adequate sleep each night.
Conclusion
In conclusion, acephalgic migraines can be debilitating, but treatments and strategies are available to help manage the symptoms. Medications, lifestyle changes, alternative therapies, and complementary treatments may all play a role in reducing the frequency and intensity of your episodes.
Additionally, avoiding common triggers and practicing self-care techniques can help to reduce the likelihood of triggering an episode. Ultimately, it is vital to work with your doctor to develop an individualized plan of care that best suits your needs and preferences.
IF YOU HAVE HEADACHE, MIGRAINE, OR FACIAL PAIN AND ARE LOOKING FOR ANSWERS ON ANYTHING RELATED TO IT, A HEADACHE SPECIALIST IS HERE TO HELP, FOR FREE!
FIRST, LET’S DECIDE WHERE TO START:
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR THE LATEST INFORMATION, HOT TOPICS, AND TREATMENT TIPS, VISIT OUR FREE BLOG OF HOT TOPICS AND HEADACHE TIPS HERE. THIS IS WHERE I WRITE AND CONDENSE A BROAD VARIETY OF COMMON AND COMPLEX MIGRAINE AND HEADACHE RELATED TOPICS INTO THE IMPORTANT FACTS AND HIGHLIGHTS YOU NEED TO KNOW, ALONG WITH PROVIDING FIRST HAND CLINICAL EXPERIENCE FROM THE PERSPECTIVE OF A HEADACHE SPECIALIST.
IF YOU DON’T HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR POSSIBLE TYPES OF HEADACHES OR FACIAL PAINS BASED ON YOUR SYMPTOMS, USE THE FREE HEADACHE AND FACIAL PAIN SYMPTOM CHECKER TOOL DEVELOPED BY A HEADACHE SPECIALIST NEUROLOGIST HERE!
IF YOU HAVE AN EXISTING HEADACHE, MIGRAINE, OR FACIAL PAIN DIAGNOSIS AND ARE LOOKING FOR FURTHER EDUCATION AND SELF-RESEARCH ON YOUR DIAGNOSIS, VISIT OUR FREE EDUCATION CENTER HERE.