Understanding Chiari Malformation Headache Symptoms and Effective Treatments
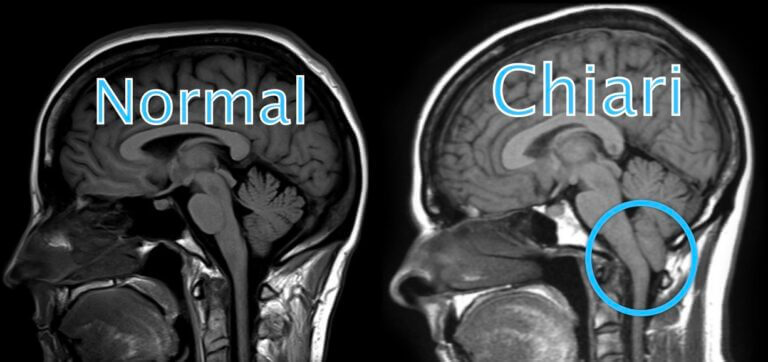
What Is Chiari Malformation? Chiari malformation, also known as Arnold-Chiari malformation, is a common congenital (born with it) condition of anatomical variation involving the brain
