Gepants (Nurtec, Qulipta) vs. CGRP Monoclonal Antibodies (Emgality, Ajovy, Vyepti, Aimovig) for Migraine Prevention
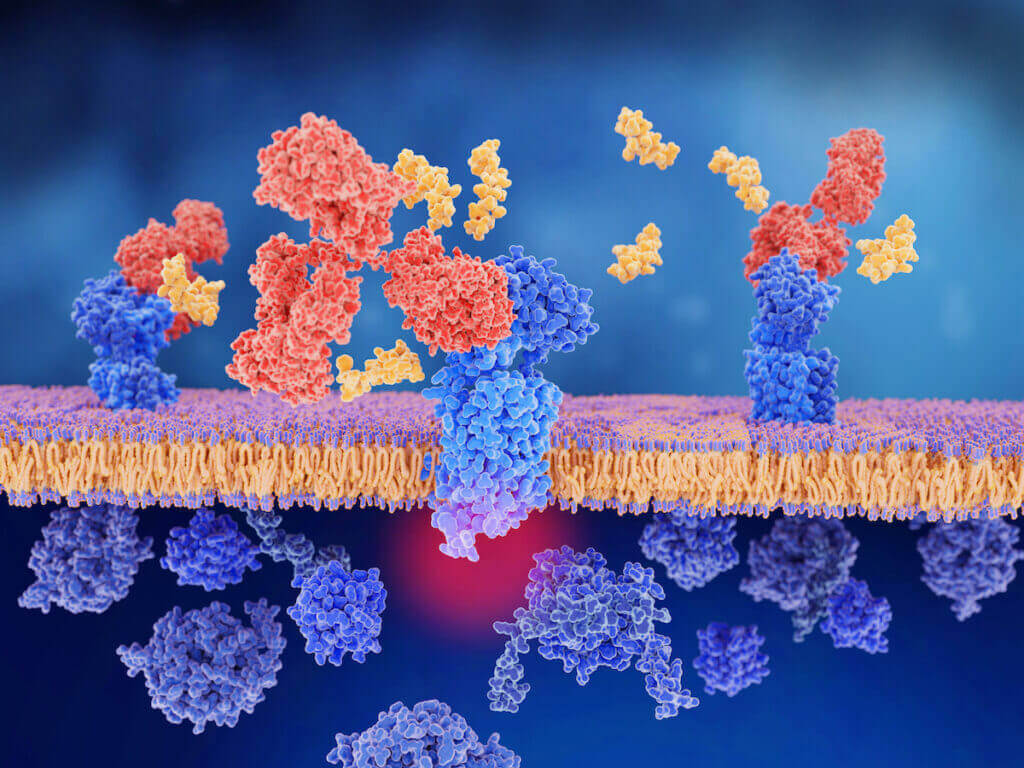
Gepants (Nurtec, Qulipta) vs. CGRP monoclonal antibodies (Emgality, Ajovy, Vyepti, Aimovig) for migraine prevention? Which medication class works better? The gepants (Nurtec, Qulipta) and calcitonin