
Can Lack of Sleep Cause Headaches?
Introduction to Lack of Sleep and Headaches Scientific studies have consistently shown that missing a good night’s sleep can lead to a variety of physical

Introduction to Lack of Sleep and Headaches Scientific studies have consistently shown that missing a good night’s sleep can lead to a variety of physical

Migraine Mastery: 5 Pillars of Migraine Control to Reclaim Your Life Reclaim YOUR Life From The Grip Of Migraine Ready to STOP missing out on

What are Migraine Glasses? When migraines intrude on daily life, the search for effective relief becomes a priority. Sometimes that relief may come from something

Understanding Migraines Migraine headaches are complex neurological events that go beyond the scope of typical headaches. As you’ve likely experienced, the intense pain of a
Migraine and Sleep Relations Migraines are severe headaches which are very disruptive to the lives of those who suffer from them. As if the headaches

Are you one of the millions of people who suffer from migraines? Have you ever considered the impact that your gut health may have on

Do you often find yourself waking up with a headache in the morning? It can be a frustrating and debilitating way to start your day.

Have you ever experienced dizziness without the classic throbbing pain of migraine headaches? Can migraines cause dizziness without pain? Is there such a thing as

I see patients stuck in the dark lonely rut of chronic migraine all day every day. Chronic migraine is a miserable headache disorder which causes
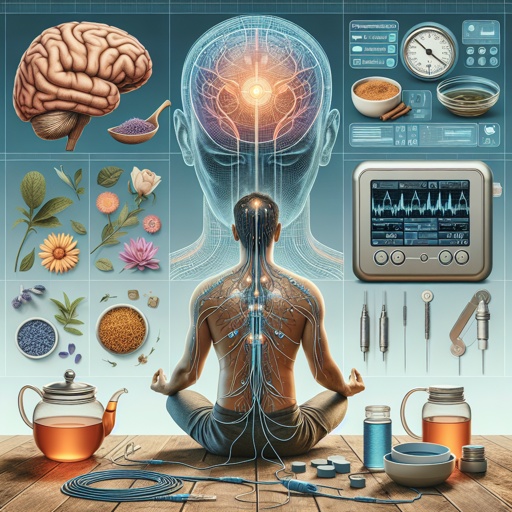
Are you tired of relying on traditional prescription medications to manage your migraine headaches, or do you get every side effect listed on the package